Waist-to-Hip Ratio, Waist Circumference and BMI
What to use for health risk indication and why.

The ever-increasing worldwide obesity epidemic is putting more and more people at risk for coronary heart disease, hypertension, abnormal cholesterol, diabetes mellitus, sleep apnea and certain cancers (Hainer, Toplak & Mitrakou 2008). However, health risks associated with obesity are of greater concern depending on the pattern of fat distribution in the body (e.g., in the torso and abdomen versus the hips, thighs and buttocks) (Srikanthan, Seeman & Karlamangla 2009).
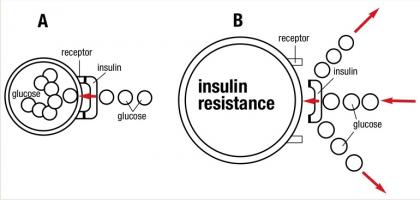
Torso and abdominal fat, referred to as visceral, central or intra-abdominal fat, is related to various health issues, including insulin resistance (see Figure 1) and abnormal blood lipid levels, which escalate the risk of diabetes mellitus and cardiovascular disease, respectively (Ness-Abramof & Apovian 2008). Presently, body mass index (BMI), waist circumference and waist-to-hip ratio are employed for classifying obesity and the risks of abdominal fat accumulation.
For fitness professionals, the important question (in addition to which body composition technique is best for tracking body fat and muscle change—skinfolds, bioelectrical impedance or hydrostatic weighing) is which anthropometric assessment is most suitable for detecting cardiovascular and metabolic risk in clients.
In the human body, fat can be divided into two main compartments—visceral (torso) and subcutaneous (under the skin). Additionally, fat is stored in smaller amounts in the heart, pancreas and liver, and within muscle, where it is referred to as intramuscular fat (which is used for fuel during exercise). Visceral body fat helps maintain blood levels of free fatty acids (triglyceride molecules separated from their glycerol “backbone”) and facilitates regulation of blood insulin (Ness-Abramof & Apovian 2008).
Visceral fat may be infiltrated by specific immune cells (known as macrophages), which trigger insulin resistance, a precursor for prediabetes and diabetes (Attie & Scherer 2009). It is meaningful to note that people with prediabetes can often prevent or delay diabetes by losing modest amounts of weight and exercising more—for example, walking 30 minutes a day 5 days a week. Losing 5%–7% of body weight can prevent or delay diabetes “by nearly 60 percent” (U.S. Department of Health and Human Services 2008).
Fat cells, once considered to be solely energy depots, are now known to be busy endocrine (hormone-secreting) organs. They secrete a number of specialized proteins known as cytokines, which regulate responses to infection, immune reactions, inflammation and trauma. In regard to inflammation regulation (i.e., the response of the body to injury or irritation), fat cells secrete pro-inflammatory (causing inflammation) and anti-inflammatory (inhibiting inflammation) cytokines (Dinarello 2000).
Some of the cytokines promoting inflammation are tumor necrosis, interleukin-6 and C-reactive protein (CRP). When chronically elevated in the circulatory system, as happens with high blood pressure, these pro-inflammatory cytokines can damage arterial walls and become the starting point for atherosclerotic plaque buildup. Elevated CRP level is positively correlated to cardiovascular disease and relatively easy to test for in a blood assay (called a high-sensitivity CRP, or hsCRP). Personal trainers should encourage clients to have their CRP assessed at the same time they have their cholesterol checked.
Fat cells also produce and secrete adiponectin, a specialized protein that improves insulin sensitivity (the cell’s ability to use glucose) and protects against atherosclerosis. Unfortunately, with visceral fat obesity accumulation, adiponectin levels fall, leading to a higher cardiometabolic health risk (e.g., higher risk of heart disease and diabetes) (Ness-Abramof & Apovian 2008).
Importantly, elevated levels of blood cortisol intensify central fat deposition. Cortisol is a stress hormone, and thus chronic stress can directly increase visceral fat accumulation. This is a good reason why mind-body classes, which help to neutralize stress, can directly counteract central fat accumulation.
BMI
BMI is calculated as weight in kilograms divided by the square of height in meters. Another simple BMI calculation is body weight in pounds multiplied by 703 and then divided by the square of height in inches. Luckily, there are many BMI calculators on the Web. The World Health Organization (WHO) has established guidelines for normal (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2) and obese (>30 kg/m2) adults.
One drawback of using BMI with fitness populations is that a muscular person will score higher, which can produce an inaccurate assessment of overweight or obesity. On the other hand, Ness-Abramof and Apovian (2008) indicate that in older populations, who tend to lose muscle mass, BMI may be underestimated. Srikanthan, Seeman and Karlamangla (2009) add that age-related changes in standing posture can inaccurately cause BMI to increase by 1.5 kg/m2 in men or 2.5 kg/m2 in women, despite minimal change in body weight. What’s more, BMI is a weak predictor of weight-related health problems among some racial and ethnic groups, such as African-American and Hispanic-American women (National Institute of Diabetes and Digestive and Kidney Diseases 2008).
Waist Circumference
Precise measurement of visceral fat requires the use of magnetic resonance imaging or tomography, which are scientific techniques that visually depict the internal tissue compositions. Waist circumference is a substitute technique for these scientific assessments. A waist circumference > 35 inches (88 centimeters [cm]) in women or > 40 inches (102 cm) in men is associated with higher cardiometabolic risk (Ness-Abramof & Apovian 2008). Welborn and Dhaliwal (2007) indicate that waist circumference is superior to BMI in predicting cardiovascular disease risk.
One practical question to ask is how waist circumference should be measured. Landmarks include the umbilicus, the midpoint between the lowest rib and the iliac crest, and just above the iliac crest. Advantageously, Ross et al. (2008) showed that all these waist circumference landmarks are equally effective in identifying all-cause mortality, cardiovascular disease and diabetes risk. So exercise professionals are encouraged to use the anatomical landmark that works best with their clients.
The measurement should be taken at the end of expiration, when the diaphragm is in its neutral position; during an inspiration the diaphragm descends into the abdominal cavity, enlarging the waist circumference measurement. A spring-loaded tape measure is recommended (use any Web search engine to obtain one), as the tension in this simple, inexpensive tool remains constant, providing consistency across all anthropometric measurements.
Waist-to-Hip Ratio
With waist-to-hip ratio, the waist is measured at its narrowest part, between the lowest rib and the iliac crest, and the hip circumference is taken at the widest area of the hips, at the greatest protuberance of the buttocks. The next step is simply to divide the waist measurement by the hip measurement. The WHO defines ratios of > 9.0 in men and > 8.5 in women as decisive benchmarks for metabolic syndrome. Welborn and Dhaliwal (2007) and Srikanthan, Seeman and Karlamangla (2009) confirm this and cite several other investigations that show waist-to-hip ratio being the superior clinical measurement for predicting cardiovascular disease risk.
It is inspiring that there is a plethora of research on these anthropometric measurements. BMI is a reliable way to tell if body weight is putting a person at generalized health risk. Waist circumference and waist-to-hip ratio are measures of central adiposity that appear to predict cardiovascular and diabetes risk better than BMI does (Srikanthan, Seeman & Karlamangla 2009).
Much research denotes that waist-to-hip ratio is the superior health risk–categorizing indicator. Many fitness professionals are highly skilled at body composition measurement techniques, such as skinfolds. In completing and explaining the anthropometric and body composition measures for clients, professionals can provide supplementary educational information about reducing cardiometabolic health risks and improving quality of life. n
A. With effectual glucose metabolism, insulin reacts with receptors on muscle, fat and the liver like a “key fitting into a lock,” opening the passageway for glucose to enter and be used by the cell.
B. Insulin resistance is a condition in which the body produces insulin but the muscle, fat and liver cells do not react with it, and the glucose cannot enter the cell. The pancreas unsuccessfully tries to resolve the problem by producing more insulin. The result is excess glucose buildup in the bloodstream, an antecedent to diabetes. Thus, most people with insulin resistance have high levels of insulin and glucose circulating in their blood.
Source: U.S. Department of Health and Human Services (2008).
Although there are age-specific table cutoffs for waist circumference in youth, Maffeis, Banzato and Talamini (2008) recommend the use of waist-to-height ratio with ≤ 0.5 being normal and > 0.5 indicating an increased metabolic and cardiovascular risk. Waist-to-height ratio is calculated by dividing a person’s waist measurement (inches) by their height (inches). Waist is measured at the narrowest point of the midsection, between the bottom rib and the top of the hip bone.
References
Dinarello, C.A. 2000. Proinflammatory cytokines. Chest, 118 (2), 503–508.
Hainer, V., Toplak, H., & Mitrakou, A. 2008. Treatment modalities of obesity: What fits whom? Diabetes Care, 31 (Suppl. 2), S269–77.
Maffeis, C., Banzato, C., & Talamini, G. 2008. Waist-to-height ratio, a useful index to identify high metabolic risk in overweight children. Journal of Pediatrics, 152 (2), 207–13.
National Institute of Diabetes and Digestive and Kidney Diseases. 2008. Weight and waist measurement: Tools for adults. http://win.niddk.nih.gov/publications/tools.htm#circumf; retrieved June 26, 2010.
Ness-Abramof, R., & Apovian, C. M. 2008. Waist circumference measurement in clinical practice. Nutrition in Clinical Practice, 23 (4), 397–404.
Ross, R., et al. 2008. Does the relationship between waist circumference, morbidity and mortality depend on measurement protocol for waist circumference? Obesity Reviews, 9 (4), 312–25.
Srikanthan, P., Seeman, T.E., & Karlamangla, A.S. 2009. Waist-hip-ratio as a predictor of all-cause mortality in high-functioning older adults. Annals of Epidemiology, 19, 724–31.
U.S. Department of Health and Human Services. National Institutes of Health 2008. Insulin resistance and pre-diabetes. NIH Publication No. 09–4893.
Welborn, T.A., & Dhaliwal, S.S. 2007. Preferred clinical measures of central obesity for predicting mortality. European Journal of Clinical Nutrition, 61, 1373–79.
World Health Organization. BMI classification. http://apps.who.int/bmi/index.jsp?introPage=intro_3.html; retrieved June 26, 2010.
Len Kravitz, PhD
Len Kravitz, PhD is a professor and program coordinator of exercise science at the University of New Mexico where he recently received the Presidential Award of Distinction and the Outstanding Teacher of the Year award. In addition to being a 2016 inductee into the National Fitness Hall of Fame, Dr. Kravitz was awarded the Fitness Educator of the Year by the American Council on Exercise. Just recently, ACSM honored him with writing the 'Paper of the Year' for the ACSM Health and Fitness Journal.