Osteoporosis: Facts, Stats and Exercise Recommendations
Health statistics, risk factors and exercise recommendations for improving bone health.

Osteoporosis is a skeletal disorder characterized by compromised bone strength, which predisposes a person to a higher risk of fracture (Klibanski et al., 2001). Klibanski et al. continue, explaining that bone strength primarily reflects the integration of bone density (i.e., peak bone mass in relation to amount of bone loss) and bone quality (i.e., bone architecture, micro-fractures and mineralization). Osteoporosis is often categorized as either primary or secondary. Women and men, of all ages, can have primary osteoporosis, which often follows menopause in women and later in life in men (Klibanski et al).
Secondary osteoporosis, on the other hand. has been described as a result of medications, health conditions or diseases (Klibanski et al., 2001). In this column we discuss the health statistics of osteoporosis, historical roots of osteoporosis, risk factors of osteoporosis, the pathogenesis of osteoporosis-related fractures, overall exercise recommendations for improving bone health, and strength training programming that best manages osteoporosis.
What Are the Health Statistics for Osteoporosis?
Osteoporosis is a major health concern in the US. According to data collected in 2017-2018 (CDC, 2022), 18.8% of women and 4.2% of men, ≥ 50 years of age, have osteoporosis of the femur neck (i.e., part of the bone that connects the head with the shaft) or lumbar spine. Citing several sources, the International Osteoporosis Foundation (2023) highlights that 1 in 3 women and 1 in 5 men, over age 50, will experience osteoporosis fractures in their remaining lifetimes. Although osteoporotic fractures can occur at any skeletal site, the bones most frequently affected are the hip, spine, upper arm, wrist and pelvis (Beck et al., 2017). Of these areas, the authors (Beck et al., 2017) state that hip fractures are the most devastating in terms of morbidity and mortality. The incidence and prevalence of osteoporosis is sure to continue rising, due to the aging worldwide population and sedentary lifestyles of most people, which result in a decrease in bone-loading daily activities.
What Is the History of Osteoporosis?
Osteoporosis has affected people for many centuries, affecting Egyptian women over 4,000 years ago (Stride, Patel and Kingston, 2013). However, it is within the last three centuries that the disease has been recognized and quantified. Back in 1754, John Hunter, a Scottish anatomist and surgeon, initiated his research on bones and teeth (Meikle, 1997; Stride, Patel and Kingstron, 2013). From his experiments and observations, Hunter was able to make some notable contributions to our understanding of the mechanisms of bone growth. Hunter discovered what is now referred to as bone remodeling, the process by which new bone is laid down in the body and the old bone is resorbed. Years later, Sir Astley Cooper, surgeon and anatomist, recognized that the age-related decline in bone density increased the risk of fracture. Years later (1830s), French pathologist Jean Lobstein is credited with introducing the term ‘osteoporosis’ or porous bone to describe what he thought (incorrectly) were holes in bones. A century after Lobstein, Albright and colleagues advanced our knowledge of osteoporosis by observing a deficiency of osteoblasts in the affected bone (Stride, Patel and Kingstron, 2013).
See also: Having the Bone Health Talk With Clients
What are the Risk Factors to Osteoporosis?
Sozen, Oziski and Basaran (2017) describe osteoporosis as a silent disease, until the patient experiences a fracture. In hopes to prevent a fracture at any major skeletal site (i.e., spine, hip, wrist, or shoulder in an adult older than 50 years) Fitness Pros should be aware of possible risk factors of osteoporosis. For example, some environmental risk factors include loose throw rugs, low level lighting, lack of assistive devices and obstacles in the walking paths (Sozen, Oziski and Bararan, 2017). Several medical risk factors for osteoporosis include poor vision, dehydration, vitamin D insufficiency, malnutrition, depression, fear of falling and diminished cognition (Sozen, Oziski and Bararan, 2017). See Figure 1 for examples of clinical risk factors to osteoporosis and fractures.
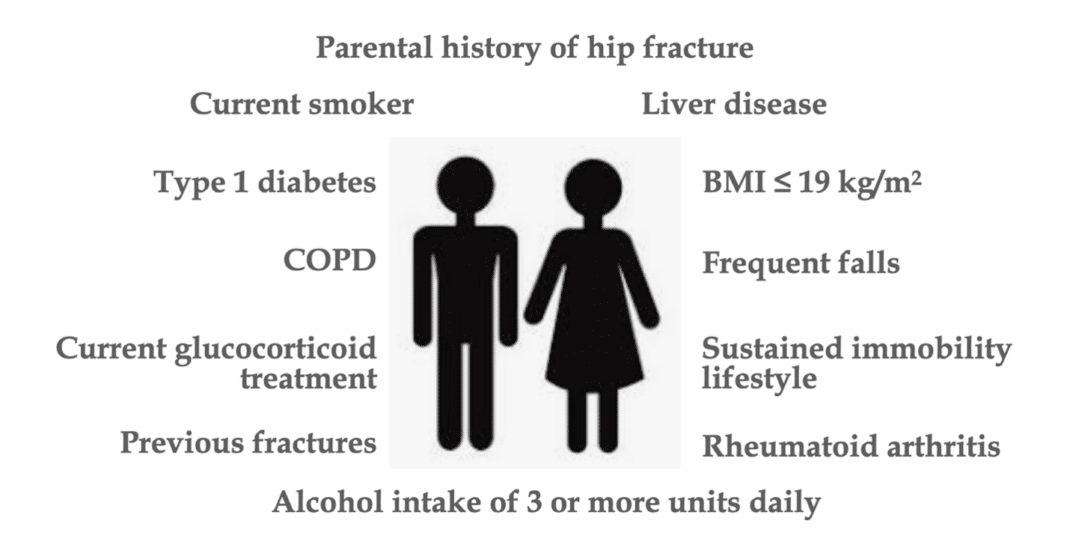
Source: Sozen, Oziski and Basaran (2017).
What Is the Pathogenesis of Osteoporosis-Related Fractures?
Pathogenesis is the process by which a disease or disorder develops. It shows the factors which contribute not only to the onset of the disease, but also to its progression and maintenance. Thus, with disease treatment interventions, scientists must first learn pathogenesis of the disease to design optimal interventions. Figure 2 shows the pathogenesis of osteoporosis-related fractures, from aging and clinical risk factors.
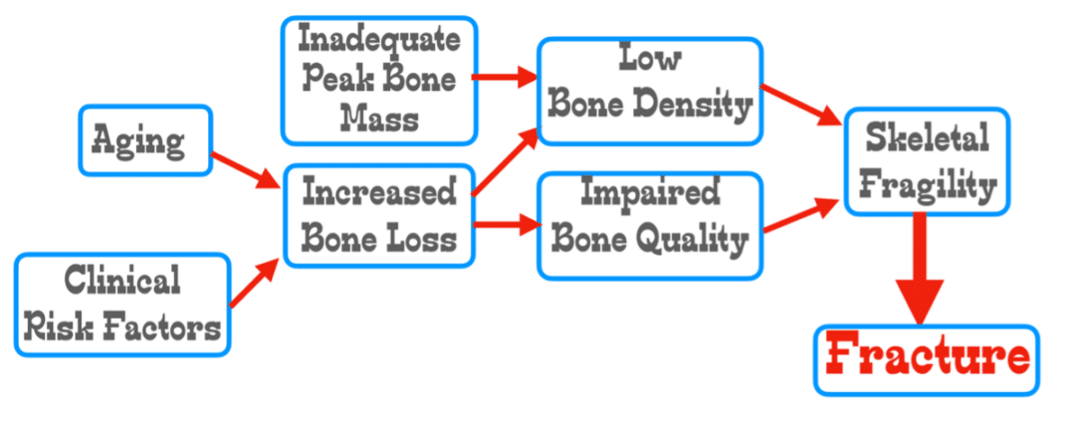
Source: Adapted from Sozen, Oziski and Bararan, 2017.
Are There Any Overall Exercise Recommendations for Improving Bone Health?
The overall exercise recommendations for improving bone health in adolescents, children, pre- and post-menopausal women and older men include the following details: exercise training should be weight-bearing, impact exercise, such as hopping, jumping, skipping and progressive resistance training (alone or in combination) (Beck et al., 2017). The researchers explain that diverse loading patterns may be particularly important for effective stimulation of bone in older adults who are not able to tolerate high magnitude impact loads. Additionally, Beck and colleagues (2017), suggest that bone adapts to customary patterns of loading (i.e., such as running). Therefore, the diversification of loading stimuli is needed to optimize the musculoskeletal system response.
See also: Exercise for Osteoporosis
What Are the Strength Training Recommendations for Osteoporosis Management?
The following resistance training recommendations are from the recent Australian position statement paper on exercise prescription for the prevention and management of osteoporosis (Beck et al., 2017).
Exercise Selection: Select 8 exercises per session, targeting major muscle groups attached to the hip and spine. For example, weighted lunges, hip abduction/adduction, knee extension/flexion, plantar-/dorsi-flexion, back extension, reverse chest flys and abdominal exercises. Some compound movements, such as squats and deadlifts are also good exercise choices.
Intensity: High to very high (80–85% 1RM; ≥16 on Borg 6–20 point RPE scale or ‘Very hard’ subjective assessment)
Frequency: 2 days/week
Sets/Repetitions: 2–3 sets of 8 repetitions
Special Exercise Considerations:
- Consider including high velocity (rapid) progressive resistance training exercises to enhance muscle power and function.
- Avoid loaded deep forward spine flexion.
- Avoid fast twisting movements of the spine.
- Emphasize good sitting and standing posture.
- Include scapular retraction, depression and back extension exercises.
- Modify sports and daily activities that involve deep spinal flexion (i.e., golf, bowling, gardening, vacuuming).
- Bend knees rather than spine to pick up or reach low objects.
Take-Home Message to Fitness Pros
Each individualized resistance exercise program for osteoporosis prevention should be aware of the following risk factors: age, frailty, loss of muscle mass, family history of osteoporosis, presence of back pain or osteoarthritis, history of fractures and falls, presence of disease(s), menopause status (women), testosterone status (men), drug use, dietary calcium and vitamin D intake, alcohol intake, smoking status and daily physical activity (Beck et al., 2017). Further, by incorporating the Special Exercise Considerations into a gradually increasing total body progressive resistance training program, you’re certain to make a big difference in the lives of your clients.
6 Relevant Questions and Answers About Osteoporosis
1. Is it too late to start an osteoporosis prevention exercise for female clients who are post-menopausal?
Answer: No, recent longitudinal data indicates that it’s never too late to start, as exercise training may prevent fracture for post-menopause clients (Beck et al., 2017).
2. What is the percent increase in mortality associated with hip fractures?
Answer: There is a 15% to 20% increase in mortality rate within one year (Sozen, Oziski and Bararan, 2017).
3. In regard to fall prevention, what conditions should fitness pros be aware of when working with older clients?
Answer: Older clients who have had a stroke or are taking medications that decrease mental alertness are particularly predisposed toward falls (Sozen, Oziski and Bararan, 2017).
4. What percent of people require long-term nursing care after a hip fracture?
Answer: About 20% to 50% of hip fracture patients require long-term nursing care. They often suffer from depression, decreased quality of life, social isolation and loss of self-esteem (Sozen, Oziski and Bararan, 2017).
5. Is there any association with caffeine intake and fracture risk?
Answer: Yes, there is some research suggesting too much caffeine intake increases fracture risk (Sozen, Oziski and Bararan, 2017).. Clients are encouraged to limit their caffeine intake to less than 1 to 2 servings (8 to 12 ounces in each serving) of caffeinated drinks per day.
6. My older clients prefer to only do walking programs. What is the evidence that walking, in and of itself, will minimize the risk of osteoporosis?
Answer: Despite the benefits of walking on aerobic fitness, fat loss, and cardiometabolic health, simply walking (for the exercise stimulus) is insufficient to optimize bone health (Beck et al., 2017).
7. Is it true that older adults are more vulnerable to falls when they do dual tasking activities?
Answer: Yes, Beck et al. (2017) submit that older adults have more falls when their attention is divided by dual tasking (e.g., walking whilst maintaining a conversation), so be careful with this type of approach.
References
Beck, B., Daly, R., Fiatarone Singh, M., & Taaffe, D. (2017). Exercise and Sports Science Australia (ESSA) position statement on exercise prescription for the prevention and management of osteoporosis. Journal of Science and Medicine in Sport, 20(5), 438-445.
CDC. (2022). Osteoporosis. Accessed July 7, 2024: https://www.cdc.gov/nchs/fastats/osteoporosis.htm
International Osteoporosis Foundation. (2023). Epidemiology. Accessed July 8, 2024: https://www.osteoporosis.foundation/health-professionals/fragility-fractures/epidemiology
Klibanski, A, Adams-Campbell, L., Bassford, T., et al. (2001). Osteoporosis Prevention, Diagnosis, and Therapy, Journal of the American Medical Association, 285(6), 785-795.
Meikle, M. (1997). Control mechanisms in bone resorption: 240 years after John Hunter. Annals of the Royal College of Surgeons of England, 79, 20-27.
Stride, P.J.O., Patel, N., & Kingston, D. (2013). The history of osteoporosis: Why do Egyptian mummies have porotic bones? Royal College of Physicians, 43, 254-261.
Len Kravitz, PhD
Len Kravitz, PhD is a professor and program coordinator of exercise science at the University of New Mexico where he recently received the Presidential Award of Distinction and the Outstanding Teacher of the Year award. In addition to being a 2016 inductee into the National Fitness Hall of Fame, Dr. Kravitz was awarded the Fitness Educator of the Year by the American Council on Exercise. Just recently, ACSM honored him with writing the 'Paper of the Year' for the ACSM Health and Fitness Journal.
Daisy Guadian
Daisy Guadian is a 4th-year Biology student at the University of New Mexico, Albuquerque. Her professional goal is to become a DPT where she can work with patients of all ages to help them recover from injuries and manage long-term medical conditions.






