Yoga for Diabetes
Learn how yoga can assist in the management of diabetes.

Prologue – From the moment she was diagnosed with diabetes, Alyssa’s life revolved around regular checkups, timely medication and rigorous dietary restrictions. As a person with a chronic metabolic condition, constantly worrying about her blood sugar levels took a toll on her mental health as well.
Before seeing the exciting result of Alyssa’s journey, let’s explore some of the background science related to diabetes and the use of yoga as an intervention.
What is Diabetes?
When we eat and digest food, the carbohydrate portion is broken down into sugar (i.e., glucose). When this glucose is absorbed into bloodstream the pancreas will secrete insulin to help the sugar pass into tissues—where it is used as energy or stored.
Type 1 Diabetes:
When the pancreas is not able to produce enough insulin to maintain healthy blood sugar levels, the pathology is called type 1 diabetes. In this type of diabetes, the pancreatic beta cells—those that produce insulin—are destroyed due to an autoimmune condition, causing excess glucose in the blood.
Type 2 Diabetes:
When the body is unable to properly use the insulin to maintain healthy blood sugar levels the pathology is known as type 2 diabetes. Type 2 diabetes is characterized by insulin resistance, which means that tissues are less responsive to insulin, and as a result, excessive levels of this hormone are needed to deal with blood sugar. To overcome this reduced insulin sensitivity the pancreas initially ramps up insulin production. Eventually, however, the pancreas is unable to keep up with this increased demand, leading to chronically higher blood sugar levels. Type 2 diabetes is also known as non-insulin-dependent diabetes (NIDDM) and it is significantly more prevalent, accounting for 90% of all diabetes (IDF 2021).
In both of the above types, diabetes leads to raised blood sugar levels which could—if left untreated—cause the failure of organs.
Gestational Diabetes:
A third type of diabetes is exclusive to pregnancy. More specifically, the hormones produced during pregnancy can cause insulin resistance. When this insulin resistance progresses it becomes gestational diabetes, which usually resolves after pregnancy. In some cases, however, it can lead to long-term complications affecting the health of the baby and the mother.

Risk Factors for Diabetes:
Type 1:
- Family history of diabetes
- Age: one is more like to get diabetes as a child, teenager or young adult
Type 2:
- Obesity
- High Blood Pressure
- Physical Inactivity
- Stress
According to the International Diabetes Federation (IDF), 1 in 10 adults suffer from diabetes, which translates to 537 million adults (20-79 years) around the globe. Projections indicate that this figure will increase to 643 million by 2030, and further to 783 million by 2045. One person dies every 5 seconds from diabetic complications, which translated to 6.7 million deaths in 2021. This rise in type 2 diabetes rates correlates with increased urbanization, aging populations, inadequate physical activity, and greater consumption of unhealthy foods (IDF 2021).
Diabetes-related expenditure accounts for 11.5% of the total global healthcare budget, and on average, individuals with diabetes spend around $3300 to $4600 USD a year on medication and doctor visits—which is about 6-8% of an average American’s yearly salary (IDF 2021; Nguyen 2023). According to projections by the IDF (2021), by 2030 total global diabetes-related health expenditure will reach 1 trillion USD.
As costs related to diabetes care soar, for both the nation and individuals, it is essential to implement preventive strategies and explore alternative cost-effective ways of managing diabetes.

How Yoga helps in the Prevention and Management of Diabetes Mellitus
Yoga is a holistic healing modality utilizing physical postures (asana), deep breathing (pranayama) and mindfulness meditation practices (dhyana) to harmonize the body, mind and emotions. There is growing scientific evidence highlighting the profound benefits of yoga on the psycho-neuro-endocrine and immune mechanisms associated with diabetes. A systematic review of controlled trials on yoga for adults with type 2 diabetes patients summarized that “yogic practices may promote significant improvements in several indices of importance in DM2 [type 2 diabetes] management, including glycemic control, lipid levels, and body composition” (Innes and Selfe 2016). Yoga is proving to be a cost-effective, non-invasive way of lowering fasting blood glucose levels, reducing oxidative stress, and enhancing the quality of life of diabetic patients (Gowri et al. 2022).
- Improves pancreatic function and reduces blood sugar levels: In a novel study of its kind, Manjunath and others (2005) set out to investigate the impact of yoga-based twists and other asanas (physical postures) on the pancreas and insulin secretion. They found that a progressive, long-term practice of asanas led to pancreatic beta cells becoming more sensitive to glucose signals (Manjunatha et. al 2005). Another study by Malhotra and others (2004) noted a marked reduction in insulin resistance after 40 days of yoga practice. They also reported that a regular yoga practice brought down high levels of insulin in obese type 2 diabetic patients, which suggested “better utilization and metabolization of glucose from peripheral tissues and the liver” (Malhotra et al. 2004). In a study by Nagarathna and colleagues (2012), 277 patients with Type 2 diabetes underwent a yoga-based lifestyle modification program over 9 months. Significant reductions in glycosylated blood sugar levels (HBa1c; a marker of long-term blood sugar regulation) and postprandial (i.e., after a meal) blood glucose were observed (Nagarathna et al. 2012).
- Weight loss: Yoga is a slow-paced, low-impact form of exercise that makes it ideal for diabetic patients who may be overweight and have limited mobility. Weightloss can help reduce insulin resistance(ADA n.d.).Yoga helps increase muscular glucose use, which can ultimately contribute to weight loss. Two comparable yoga intervention studies—one conducted in India and the other in Korea—reported significant reductions in body weight, body mass index, and total cholesterol levels among individuals with type 2 diabetes (Gowri et al. 2022; Seo et al. 2012). The Indian study (Gowri et al. 2022) highlighted that the reduction of fat from the waist pointed to a redistribution of fat which could be due to a change in insulin resistance. Another study found that yoga led to a greater decrease in waist circumference compared to a control group, which participated in walking (McDermott et al. 2014).
- Effective stress management technique: Stress has been associated with the release of hormones like epinephrine (aka adrenaline) and cortisol that result in elevated glucose levels (Yaribeygi et al. 2022). Chronically high levels of these stress hormones can lead to binge eating and intra-abdominal fat buildup, which in turn contribute to insulin resistance and a heightened risk of heart attacks (McCall 2007). The more chronically stressed a diabetic person becomes, the greater the potential for their blood sugar levels to shoot higher, subsequently raising the risk of serious heart complications.
In another study, researchers set out to determine if a stress management training program could improve glucose metabolism in patients with diabetes (Surwit et al. 2007). They measured the HbA1c levels and used the Spielberger State-Trait Anxiety Inventory, Perceived Stress Scale and the General Health Questionnaire, to measure levels of stress. The study participants were offered training which included guided imagery, meditation and deep breathing along with progressive tensing and relaxation of muscles. At the end of one year, the HbA1c levels of participants who received stress management training were significantly lower than those of the control group (Surwit et al. 2007).
Collectively, the growing scientific evidence indicates that yoga’s effectiveness in reducing stress could potentially moderate the impact of diabetes.
Epilogue – Alyssa went to her first yoga session to help her lose weight. She was about 100 pounds overweight and had difficulty walking or running due to her knee issues. She joined yoga for its popularity as a low-impact exercise. As a software professional, she spent all of her days sitting at a desk, commuting to work, and taking care of her kids. A stressful work environment coupled with a lack of physical exercise meant she needed a yoga routine that would help manage her mental health as well.
Over six months she lost about 40 pounds. More importantly, she discovered a newfound awareness of the edge of her appetite: she became more attuned to her body’s hunger cues and signals of fullness helping her to avoid mindless overeating. This mindfulness around food also led to a sharp drop in craving for unhealthy snacks.. She also felt much calmer and better equipped to deal with her day-to-day stressors more holistically.
Therapeutic Yoga Module for Diabetes Mellitus
Asanas
Forward bends and twists focus on alternating abdominal contraction and relaxation.
Ardha Matsyendrasan (Seated Spinal Twist)

- Begin by sitting with both legs outstretched in front of you on a mat.
- Bend the right knee, crossing the right foot over the left knee and place it to the outside of the left knee.
- Bend the left knee and place it to the outside of the right hip.
- Inhaling, lengthen the spine and place the right hand behind you.
- Exhaling twist your body to the right, getting your left elbow over your left knee or hugging your right knee with your right arm.
Pachimottanasan (Forward fold)

- Sit with your legs outstretched.
- As you exhale hinge forward from the hip joint, lengthening the spine.
- You can choose to do it with a bolster on your knees for a restorative effect.
Mandukasan (Frog pose)

- Begin in Vajrasan position: sitting back on heels with knees bent, tall (erect) spine and heels separated (see Figure 3 for lower body position).
- Create a fist with both hands placing the thumbs inside and place both fists on the navel, beside the belly button.
- Inhaling, lengthen the spine.
- Exhaling, fold forward from the hips, keeping the lift in the chest.
- You can also choose to rest your forehead on a block or a pillow.
Dhanurasan (Bow pose)

- Lie flat on your belly with your forehead on the mat.
- Bend your knees and hold your ankles. (If you can’t reach your ankles, you can loop a belt around the ankles and grab the belt).
- Inhaling, lift the thighs and chest off the mat.
- Exhaling, gently release the ankles to get the legs and chest back down on the mat.
Supported Setu Bandhasan (Bridge pose)
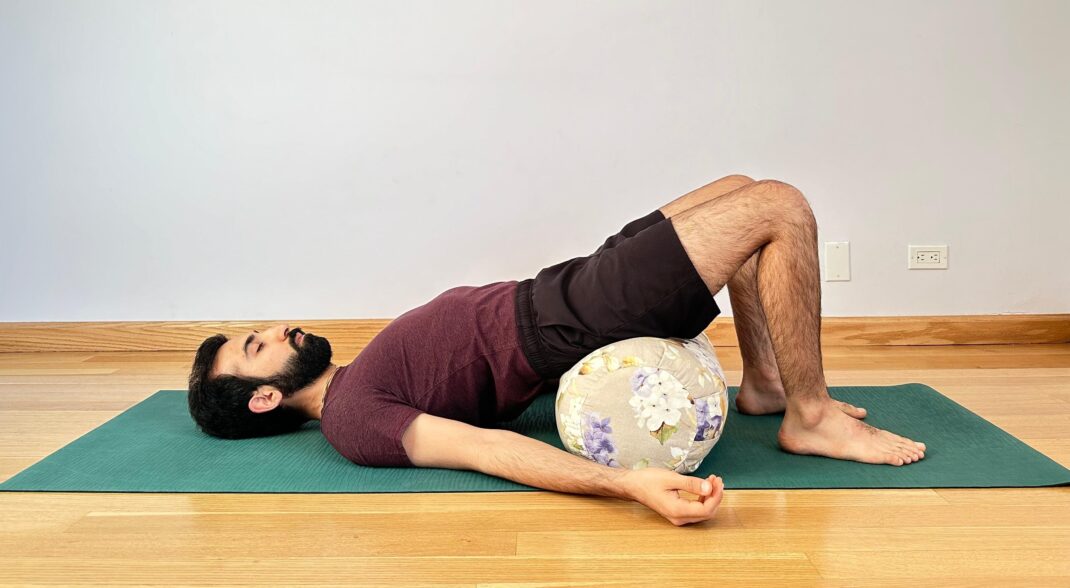
- Being by lying on your back with your knees bent, arms beside the hips.
- Slowly raise your hips and place a bolster underneath supporting your buttocks and lower back.
- Keep breathing steadily and gently.
- Stay in the restorative position for a few minutes.
Pranayama (controlled breathing techniques)
Bhastrika* (Bellows breathing)


*Practice this pranayama with caution and under the guidance of a qualified yoga teacher or therapist.
- Sit in a comfortable cross-legged sitting posture.
- Keep the spine erect.
- Make a fist with both hands and get the fists near your shoulders.
- Inhaling, raise your arms up and open the fists.
- Exhaling forcefully, bring your hands beside the shoulders as you close your fists.
- Repeat the forceful breathing around 5-10 times.
Brahmari (Humming Bee Breath)

- Taking Shankmukhi mudra as shown in Figure 7:
- Thumbs closing the ears,
- Index fingers gently placed over your eyelids.
- Middle fingers on the side of the nose.
- Ring finger above the upper lip.
- Inhale deeply through both nostrils.
- Make a resonant, long ‘Mmmmm’ sound without straining at the end.
- Repeat for 5-10 rounds.
Special Considerations and Contraindications
Sometimes a patient’s blood glucose levels may drop soon after starting practice. It is vital to consult your doctor before making any changes in medication. Patients suffering from complications like peripheral neuropathy must be careful to never jump or make sudden movements that could lead to injury and infection. Any form of vigorous hot yoga would not be advised.
See also: Magnesium and Diabetes Risk
References
ADA (American Diabetes Association). n.d. Understanding Insulin Resistance. Accessed July 12, 2024: diabetes.org/health-wellness/insulin-resistance.
Gowri, M., et al. 2022. Impact of an Integrated Yoga Therapy Protocol on Insulin Resistance and Glycemic Control in Patients with Type 2 Diabetes Mellitus. Rambam Maimonides Medical Journal, 13 (1), 1-11.
Innes, K. E., & Selfe T. K. 2016. Yoga for Adults with Type 2 Diabetes: A Systematic Review of Controlled Trials. Journal of diabetes research. 2016 (1), 1-23.
IDF (International Diabetes Federation). 2021. IDF Diabetes Atlas. Accessed July 10, 2024: diabetesatlas.org.
Malhotra, V., et al. 2004. Effects of yoga asanas and pranayama in non-insulin dependent diabetes mellitus. Indian journal of traditional knowledge. 3 (2), 162-167.
Manjunatha, S., et al. 2005. An investigation into the acute and long-term effects of selected yogic postures on fasting and postprandial glycemia and insulinemia in healthy young subjects. Indian journal of physiology and pharmacology. 49 (3), 319-24.
McCall, T. 2007. Yoga As Medicine. New York, NY: Bantam Dell. 283.
McDermott, K. A., et al. 2014. A yoga intervention for type 2 diabetes risk reduction: a pilot randomized controlled trial. BMC complementary and alternative medicine. 14, 212.
Nagarathna, R., et al. 2012. Efficacy of yoga based life style modification program on medication score and lipid profile in type 2 diabetes—a randomized control study. International Journal of Diabetes in Developing Countries, 32 (3), 122-130.
Nguyen, A. 2023. The True Cost of Diabetes: How Much Do Patients Pay Each Year? Good Rx Health. Accessed July 10, 2024: goodrx.com/conditions/diabetes/true-cost-of-diabetes.
Seo, D. Y., et al. 2012. Yoga training improves metabolic parameters in obese boys. The Korean journal of physiology & pharmacology: official journal of the Korean Physiological Society and the Korean Society of Pharmacology. 16 (3), 175-80.
Surwit, R. S., et al. 2002. Stress management improves long-term glycemic control in type 2 diabetes. Diabetes care, 25 (1), 30-34.
Yaribeygi, H., et al. 2022. Molecular mechanisms linking stress and insulin resistance. EXCLI journal. 21, 317-334.