
The Physiology of Sprint Interval Training
If your clients haven’t already asked you about it, they will. High-intensity interval training is a mainstay in personal training programs and group fitness classes. There are several reasons why HIIT is a good workout, one of them being its brevity. Research indicates that the four most common barriers to exercise are not having time, feeling too tired, getting enough exercise at one’s job, and having no motivation to exercise (Brownson et al. 2001).
In 2008, the U.S. Department of Health and Human Services recommended that all Americans perform at least 150 minutes of moderate-intensity—or 75 minutes of vigorous–intensity—aerobic physical activity each week for substantial health benefits (Office of Disease Prevention and Health Promotion 2008). With this in mind, what can fitness professionals do to meet people where they are? HIIT may provide a solution, and it has become a very popular form of vigorous–intensity training for fitness enthusiasts.
HIIT involves repeated bouts of high-intensity exercise interspersed with recovery periods of rest or low-intensity activity (Weston, Wisløff & Coombs 2014). Weston and colleagues submit that incorporating HIIT may help clients glean health–enhancing benefits in less time, thus making this training method a time-efficient and appealing option. The researchers also conclude that HIIT may address another common limiting factor: lack of motivation, which is a common complaint clients levy against lengthy steady-state continuous exercise.
Newer research has revealed that short–burst HIIT, or sprint interval training (high–intensity bouts up to 30 seconds alternating with lower–intensity recovery periods up to 4.5 minutes), elicits meaningful cardiovascular and metabolic responses (Boutcher 2011). However, the literature has been lacking an optimal work/recovery short-burst protocol for specific physiological responses. This became a central question we wanted to address with the design of our study, exclusive to IDEA Fitness Journal readers.
Objectives of the Sprint Interval Study
Our sprint interval study was designed and conducted to investigate the metabolic (oxygen consumption, caloric energy expenditure, blood lactate, excess postexercise oxygen consumption) and cardiovascular (heart rate, postexercise blood pressure) effects of three popular interval training protocols in healthy college-aged females and males. The sprint interval protocols we tested resulted in the same total work output but differed in their work–to–recovery ratios. One definitive goal was to identify a safe and effective high–intensity interval training program that would reduce the time required for physiological improvement.
In research studies, sprint interval training programs typically involve participants performing “all out” or at a maximal-exertion intensity (Boutcher 2011). However, as Boutcher observed, this level of intensity can be extremely hard for many individuals. Therefore, to better generalize our results to the range of fitness levels in women and men, we decided to set the higher work intensities at a “hard to very hard” level (relative to each participant’s perceived exertion) in the hope that participants would find the effort challenging but more tolerable and enjoyable than going all out.
Since our primary research goal was to determine the most effective of three different sprint interval programs, we used a lower-body SPARC™ trainer made by Cybex® as our exercise mode. By choosing lower-body-only equipment, we successfully controlled for any contributions of the upper body to the physiological parameters being investigated. (In any experimental design, researchers try to control for factors that may compromise the validity of the results. Since the use of arms could have varied between the different sprint protocols and become what is referred to as a confounding variable, we chose to use a lower-body-only exercise device.)
A secondary reason for selecting the SPARC trainer was that its gliding action is designed to be less stressful on lower-extremity joints, which we felt was advantageous. By standardizing total work completed, as well as work interval intensity, in the three protocols (only the recovery varied), we hypothesized that we’d be able to determine whether an optimal short sprint interval work–to–recovery ratio exists for healthy, physically active young women and men.
Study Methods and Procedures
The details of the study are below.
Subject Demographics
Twelve healthy (n = 12 [male = 6; female = 6], weight = 155.4 ± 29.6 pounds, height = 67.3 ± 4.3 inches, body fat = 16.4 ± 6.0%) college-aged participants (aged 19–28) volunteered to participate in the study. They reported no cardiovascular, pulmonary or metabolic disorders on their health history forms. The participants followed pretest guidelines of abstaining from physical activity, caffeine and alcohol for 24 hours before all testing sessions, and provided verbal and written consent. All experimental procedures took place at the University of New Mexico exercise physiology laboratory in accordance with standards established in the World Medical Declaration of Helsinki, a set of ethical principles developed by the World Medical Association (2013) regarding human experimentation.
Exercise Testing Sessions
Exercise session 1. Each participant performed an individualized maximal aerobic capacity test on a cycle ergometer to determine VO2max (average = 40.53 ± 5.94 milliliters/kilogram/minute). We based criteria on attainment of two of the following: respiratory exchange ratio (RER) > 1.15, ± 10 beats/minute of predicted maximum heart rate (MHR = 220—age), plateau at ≤ 150 ml/minute of VO2, and ratings of perceived exertion (RPE) > 17 (6–20 scale). For clarification, the RER is the ratio between the amount of carbon dioxide produced in metabolism and the amount of oxygen used by the body. RER is an indirect measurement that shows the working muscle’s oxidative capacity to get energy, and where the fuel (fat and/or carbohydrate) is coming from.
Following the aerobic capacity test, participants were familiarized with the SPARC trainer. We encouraged them to attain a “hard to very hard” (RPE 16–17) intensity that they felt they could maintain for the 10 high–intensity bouts in each trial. Participants were then instructed to find a “light” (RPE 10–11) intensity, which became the baseline for all recovery intervals. See Figure 1 for a photo of the trial testing.
Exercise sessions 2, 3 and 4. Participants came to the same location as they did in session 1. They received a reminder call or email with the following instructions:
- Do not exercise or drink alcohol/caffeine for 24 hours before the session.
- Drink 1 pint (0.5 liters) of water 1–2 hours before the workout.
- Eat a light meal 2–3 hours beforehand.
Each participant then performed the three sprint interval protocols over a 3-week period with at least 2 days and no more than 7 days between protocols. Participants were encouraged to maintain their normal physical activity and nutrition lifestyle during the study. However, they were reminded not to do vigorous exercise or lower-body resistance training in the 24 hours prior to each trial.
The protocol test order was randomly assigned for each participant. Before the start, each person completed a 3-minute self-selected warm-up on the SPARC trainer. Testing sessions lasted 33–43 minutes and consisted of 10 bouts of the work-to-recovery ratios described below. After each trial, participants sat quietly so that we could collect 20 minutes of data on excess postexercise oxygen consumption. EPOC, often informally called the exercise afterburn, is a measure of the body’s postexercise use of oxygen to restore itself to pre-exercise levels. Higher-intensity exercise programs elicit the greatest EPOC values (Borsheim & Bahr 2003).
Each sprint interval protocol included 30–second intervals of very hard work. The 30–second work interval, also referred to as the Wingate test, is popularly used in interval training research (Boutcher 2011). Here are the protocols that were randomly assigned to the participants:
- 30/30 (short) protocol: 30 seconds of work at “hard to very hard” intensity/30 seconds of recovery at “light” intensity (10 bouts = 10 minutes test duration + 3 minutes warm–up + 20 minutes EPOC = 33 minutes total)
- 30/60 (medium) protocol: 30 seconds of work at “hard to very hard” intensity/60 seconds of recovery at “light” intensity (10 bouts = 15 minutes test duration + 3 minutes warm–up + 20 minutes EPOC = 38 minutes total)
- 30/90 (long) protocol: 30 seconds work at “hard to very hard” intensity/90 seconds of recovery at “light” intensity (10 bouts = 20 minutes test duration + 3 minutes warm-up + 20 minutes EPOC = 43 minutes total)
Trained and experienced technicians administered all exercise tests and collected all blood lactate samples. We measured blood lactate before each protocol, immediately postexercise and 20 minutes postexercise using a pinprick technique applied to the earlobe to extract a small blood sample (0.7 microliter). Oxygen consumption and heart rate were continuously collected and monitored during each training protocol and during the 20 minutes of EPOC. We also took blood pressure measurements manually before each protocol and within 30 seconds of each trial’s completion.
Statistical Analysis
We used a one-way repeated-measures ANOVA (a statistical technique) to examine differences between the three protocols. If any differences existed, we used a statistical comparison procedure called a Bonferroni test to identify sample means that were significantly different from each other. The p value (calculated probability) was set at a p ≤ 0.05 level. In statistics, this p value tells us that the results have a 95% chance of being true, and a 5% chance of not being true.
Study Results
- Mean average oxygen consumption (VO2) for each protocol, encompassing both work and rest periods, are illustrated in Figure 2. Results indicate no statistically significant differences among the protocols. However, the short protocol (30/30) elicited the greatest response. The long protocol (30/90) drew the lowest response, and the medium protocol (30/60) fell in between (Figure 2).
- Figure 3 illustrates mean respiratory exchange ratio for each protocol, encompassing both work and rest periods. RER results also show no statistical difference among protocols; however, the 30/30 protocol again elicited the greatest response (Figure 3). RER is an indicator of which fuel (carbohydrate or fat) is being metabolized to supply the body with energy. Although not significantly different, these results show that the short protocol used the most carbohydrate for fuel, followed by the long protocol and then the medium protocol.
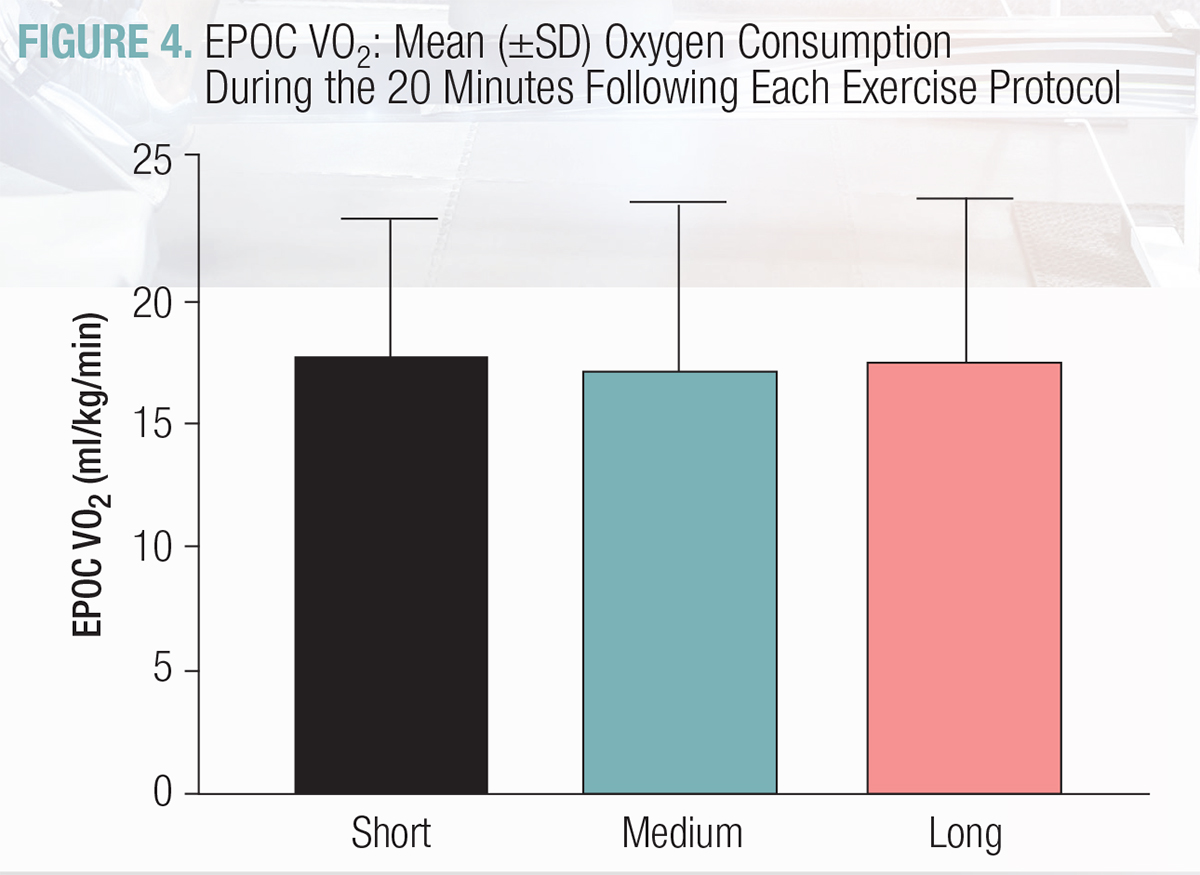
- EPOC averages are illustrated in Figure 4. Data analysis revealed no significant differences between protocols.
- Figure 5 shows the mean heart rate for each protocol, encompassing both work and rest periods. Again, there were no statistical significances among the three tests. However, 30/30 elicited the highest response (177 beats per minute), and 30/90 elicited the lowest response (170 bpm), with 30/60 falling in between (176 bpm).
- The average pre–exercise blood pressure was 114/69 millimeters of mercury (Table 1). Immediately after the short protocol, mean blood pressure was 137/74 mm Hg. Blood pressure did not significantly differ from this at the end of the medium and long protocols (136/69 and 134/70, respectively). From a clinical perspective, this is a very good finding. It clearly shows that none of these protocols presents an undesirable cardiovascular response, thus suggesting that each option may be a viable method for preventing hypertension.
- The mean blood lactate concentration for each protocol, taken immediately postexercise, is shown in Figure 6. Concentrations did not differ significantly among the protocols (either immediately postexercise or 20 minutes later). Blood lactate is an indirect measure of intensity. For instance, blood lactate after maximal exercise may range from 15 to 25 millimoles (mM), whereas the
range for these sprint protocols was well below that, suggesting that the intensities in this study were comfortably challenging. - Exercise energy expenditure per minute for the three protocols averaged approximately 10 kilocalories per minute and was not statistically different among protocols (Figure 7). Total caloric expenditure was, however, significantly higher in the 30/60 (240 ± 34 kcal) and 30/90 (277 ± 58 kcal) protocols than it was in the 30/30 (183 ± 25 kcal).
- No other SPARC-related training variables (maximum watts, average watts and average strides per minute) differed significantly among the three different sprint interval training protocols.

Take-Home Findings and Applications
- The study results clearly indicate that 30/30, 30/60 and 30/90 sprint interval training protocols, each incorporating 10 bouts of 30-second bursts of “hard to very hard” exercise, can be effective and safe physiological stimuli for healthy young female and male adults. This finding helps to validate the concept of “individualizing” workout intensity. When someone trains at an intensity relative to his or her fitness level, it results in a positive exercise stimulus and outcome.
- One decisive goal of this study was to identify an effective training program that would reduce the time required for meaningful physiological response. Such a program could help people meet U.S. Department of Health and Human Services physical activity guidelines. For the most part, the short 30/30 sprint interval protocol (with 10 bouts lasting 10 minutes) elicited cardiovascular and metabolic responses equivalent to those prompted by the 30/60 (medium) and 30/90 (long) protocols. In fact, with average oxygen consumption, the short protocol elicited the greatest response. Many personal trainers are now offering 30-minute personal training sessions for clients, making the 30/30 sprint training option quite viable.
- Two participants did not complete the study. Although we didn’t ask them why they chose to drop out, this finding is still helpful. They may have dropped out for a number of reasons (time required to complete the testing, personal issues, lack of interest in the training, etc.), and it is a meaningful reminder that people’s exercise interests vary. It therefore behooves fitness professionals to offer a variety of workout opportunities.
- The EPOC findings are somewhat surprising. Research shows that intensity and duration are meaningful factors that affect EPOC (Borsheim & Bahr 2003). However, even with precisely the same work intervals and only clear variations in recovery times, there was no significant difference in EPOC among the three protocols. Plus, these results show how elevated EPOC values (from sprint interval training) contribute positively to postworkout calorie expenditure, which is most important for weight management.
- After each sprint interval testing session, we collected an RPE from participants to find out how hard the entire workout was. The average posttraining RPE for the three protocols was 16.5 (between “hard” and “very hard” on the 6–20 RPE scale). Based on our results (with 10 high-intensity bouts in each protocol), we encourage 30–second work intervals at a “hard to very hard” intensity, combined with recovery at a “light” intensity, as these levels appear to be safe (based on blood pressure results), practical, time-efficient and effective.
- For the three protocols we tested, the total caloric expenditure values—183 ± 25 kcal for 30/30; 240 ± 34 kcal for 30/60; 277 ± 58 kcal for 30/90—indicate the very positive value these programs may bring to a weight management plan.
In summary, it’s safe to say that sprint interval training is here to stay and that it does indeed stimulate positive physiological outcomes. The key is to assess correctly, align goals with sound programming, and coach clients to work at their own pace.
1 Comments
Leave a Comment
You must be logged in to post a comment.






The figures and tables seem to be missing from the article.