Coronary Artery Disease: What Every Fitness Professional Needs to Know
Developing a thorough understanding of coronary artery disease (CAD) can help fitness professionals fight one of the world’s deadliest diseases.
How deadly? For starters, CAD is the leading cause of death around the world, accounting for 13.2% of all deaths in 2012 (WHO 2014a). It kills almost 380,000 Americans every year (CDC 2014a). Exercise professionals can do something about these statistics by designing fitness programs that reduce CAD risk factors in clients while improving their quality of life.
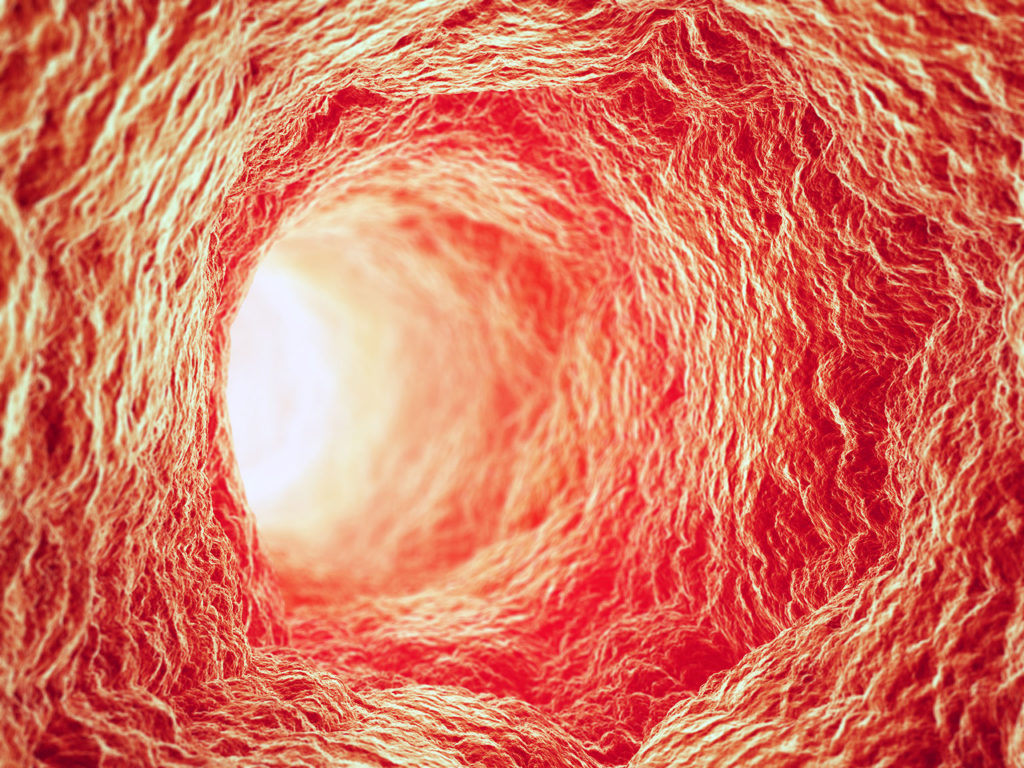
CAD results from (and is detected by) progressive accumulation of fatty plaque substances, called atherosclerosis, on the inner walls of coronary arteries (NIH 2011). The plaque restricts oxygen-rich blood to the myocardium, or heart muscles.
Note that CAD and cardiovascular disease (CVD) are not the same thing. CAD is just one variety of CVD—a cluster of diseases that include abnormal heart rhythms, heart failure, heart valve disease, congenital heart disease, heart muscle disease, pericardial disease, aorta disease and blood vessel disease.
Understanding Coronary Artery Structure and Arteriosclerosis
The heart’s coronary arteries, and all blood vessels for that matter, have three distinct layers (Hendry, Farley & McLafferty 2012) (see Figure 1):
- Tunica intima. The inner layer—the name means “inner coat” in Latin—is smooth, thin and elastic. The tunica intima is lined with endothelial cells that come in direct contact with the blood.
- Tunica media. The middle layer consists of elastic tissue intertwined with smooth muscle layers that permit contraction and dilation (the enlarging or expanding diameter of a blood vessel).
- Tunica adventitia. The tough outer layer, which is made up primarily of collagen fibers and connective tissue, provides a supportive role. The tunica adventitia anchors blood vessels to surrounding structures. This layer also keeps blood vessels from overexpanding in response to abnormally high blood pressure.
With aging, some of the larger arteries lose some of their elastic fibers and become stiffer. The inner layer becomes thicker and harder owing to a buildup of fat and calcium deposits behind it. This disease process is called arteriosclerosis (or hardening of the artery walls), which increases resistance to the flow of blood in an artery (because the artery loses some of the elasticity that allows it to expand); this often leads to a persistent elevation in blood pressure (Hendry, Farley & McLafferty 2012).
What Are the Endothelial Cells, and What Do They Do?
Endothelial cells make up the innermost lining of the tunica intima of blood vessels, maintaining a physiological equilibrium for inflammation, platelet aggregation (the sequence of events leading to the formation of a clot, or thrombosis) and blood vessel wall remodeling in response to injury (Schwartz et al. 2010). These specialized endothelial cells also regulate constriction of vessel blood flow, profoundly affecting the overall function of the cardiovascular system. Schwartz et al. (2010) explain that endothelial cell dysfunction (discussed in the next section) is an early sign of atherosclerosis.
Understanding CAD and the Pathophysiology of Atherosclerosis
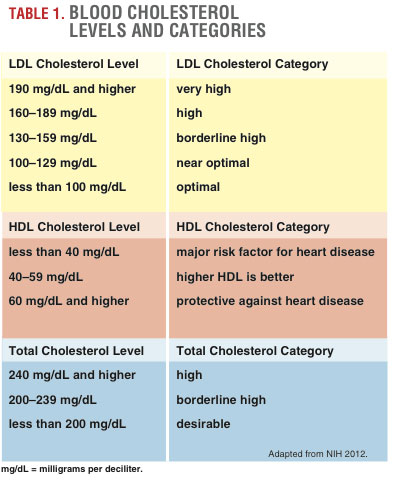
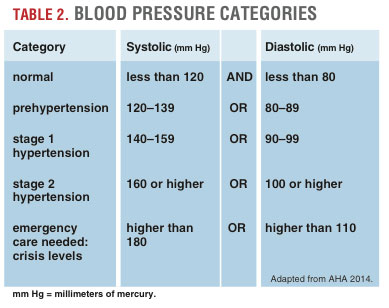
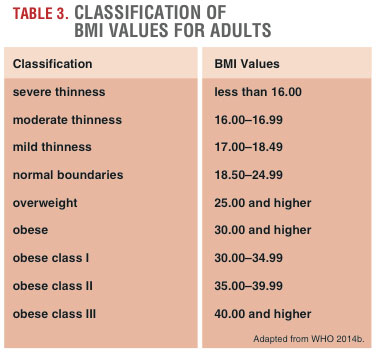
CAD occurs when atherosclerotic plaque builds up in arteries over decades (see Figure 2). In the earliest stages of the disease, chronic inflammation happens in response to damage to the endothelial lining, such as injury from chemical intrusion (e.g., elevated blood glucose, abnormal LDL cholesterol levels and/or carcinogens from tobacco or the environment) or from physical forces (e.g., high blood pressure).
Louis and Zahradka (2010) explain that chronic inflammation leads to endothelial cell dysfunction, the first step in atherosclerotic plaque formation. This dysfunction causes endothelial cells to produce less nitric oxide, hindering their major role in maintaining and controlling vascular wall functions such as muscular tone, oxidative stress and inflammation. Endothelial dysfunction also makes the tunica intima more permeable, allowing molecules to enter into and embed behind this innermost layer. Phagocytic cells, which engulf cell debris, begin to adhere to the endothelial cells in an effort to clear out some of the debris, but gradually transform into larger macrophage cells, which start to engulf LDL cholesterol molecules under the tunica intima.
The LDL cholesterol molecules oxidize; that is, each molecule loses an electron. Yang, Mohamed and Zhou (2012) explain that oxidized LDL particles are toxic and can further damage the endothelial cells. The macrophages continue to enlarge, developing into foam cells (which are fat-filled macrophages). The foam cells progressively become fatty streaks and then thicker intermediate lesions, which eventually become atherosclerotic plaque (made of smooth muscle cells, cholesterol, fatty substances, cellular debris and fibrin).
Atherosclerotic plaque significantly hinders blood flow. The plaque is surrounded by a fibrous cap that is weak and prone to rupturing. For example, a surge in blood pressure may crack a portion of the plaque. The body then sends a team of platelets to form a blood clot to stop the bleeding. This blood clot is called a thrombus. If a piece of plaque or thrombus breaks off from the tunica intima, it is known as an embolus (or thromboembolus), which will move into the bloodstream and potentially occlude smaller blood vessels downstream.
Exercise Is a Powerful Way to Combat CAD
According to Alves (2014), physical activity’s ability to reduce cardiovascular risk is as meaningful as the risk reduction from drug therapies such as cholesterol-lowering statins. Alves cites research documenting that regular exercise helps prevent CAD risk factors such as type 2 diabetes, hypertension and metabolic syndrome. In addition, Alves says, aerobic and resistance exercise can decrease blood pressure (when elevated), improve body composition, lower chronic inflammation and improve lipid profiles in overweight and obese people.
Evidence is mounting that on a molecular level, regular physical activity increases endothelial cell function (Lenk et al. 2011). Alves (2014) explains that exercise appears to mobilize specialized endothelial progenitor cells (EPCs), releasing them from bone marrow into sites of endothelial damage in response to structured physical activity. EPCs promote the regeneration and repair of a damaged endothelium.
What Are the Safe and Effective Cardiovascular Recommendations for CAD Clients?
ACSM’s Guidelines for Exercise Testing and Prescription (2014) states that exercise is safe and effective for people with CVD. These are the ACSM guidelines for developing and implementing exercise programs for a CAD client:
Medical considerations. Appropriate monitoring and exercise supervision plus communication with the client’s doctor may enhance clinical progress. Personal trainers should regularly check preexercise heart rate, blood pressure, body weight (weekly), symptoms of clinical status (lightheadedness, irregular pulse, chest discomfort, etc.), medication changes and adherence to medications. Clients may not be aware of atypical variations in their daily lives.
Duration and intensity. Exercise should be performed at least on 3 days per week and preferably on most days of the week. A 5- to 10-minute light-intensity warm-up should precede exercise sessions. Aerobic frequency depends on the client’s baseline fitness, health goals and exercise capacity. Intensity can range from 40% to 80% of the client’s heart rate reserve. Exercise heart rate should be 10 or more beats per minute below the intensity that evokes any abnormal signs or symptoms. If rating of perceived exertion is used to monitor intensity, this would be an 11 (light) to 16 (hard) on the 6–20 RPE scale.
If a client has had medical testing for exercise, the intensity is often based on a heart rate from the medical assessment. If the exercise program begins relatively soon after a cardiac-related event, the trainer may want to start the client with just 5–10 minutes of aerobic exercise.
Progression. Individualized and gradual progression should depend on the client’s fitness level, goals, motivation and other physiological limitations. The stated ACSM (2014) goal for cardiovascular conditioning is that sessions should eventually last 20–60 minutes. The new American Heart Association (AHA 2015) heart health guidelines encourage 40 minutes of moderate to vigorous exercise three to four times a week.
Equipment. To promote whole-body fitness, the ACSM guidelines encourage using a variety of exercise equipment that involves the upper and lower extremities; for example, rowers, elliptical trainers, stair climbers, recumbent steppers, upright and recumbent cycle ergometers and treadmills. Brisk walking is a very tolerable exercise and leads to fewer orthopedic problems than jogging or running.
Can CAD Clients Do High-Intensity Interval Training?
Pattyn et al. (2014) conducted a systematic review and meta-analysis of current research and found that high-intensity interval training is not only possible for CAD clients but, with respect to some physiological factors, is actually more effective than traditional moderate continuous cardiovascular training (MCT). The authors reviewed nine studies comparing HIIT and MCT with a total of 206 participants. In what may be pioneering findings, results indicated that HIIT elicits larger benefits for peak VO2 (maximal aerobic capacity) than MCT does in CAD patients.
In addition, cardiac output and stroke volume increase more after 12 weeks of HIIT than after 12 weeks of MCT. However, if weight loss is a priority, it should be noted that body weight tends to decrease more after MCT than after HIIT, according to Pattyn and colleagues (2014). This is because the capability to increase total exercise volume and duration in MCT makes it an effective strategy for enhancing weight (and fat) loss.
A word of caution about HIIT for CVD clients, from the 2014 ACSM guidelines: After highlighting and substantiating some of the impressive findings discussed above, ACSM has submitted that HIIT shows potential for people with CVD, but until further data are available regarding safety and efficacy, it cannot be universally recommended. Moreover, further research is required to determine optimal HIIT protocols for CAD clients.
Also, as a special message to personal trainers who work with CAD clients in cold, snowy regions: Shoveling wet snow can become a very physically demanding, intermittent lifestyle activity with heavy-exertion shoveling spurts alternating with recovery, similar to structured HIIT training. However, shoveling wet snow may undesirably elevate heart rate and blood pressure, placing undue stress on the cardiovascular system.
Can CAD Clients Do Resistance Training?
Resistance training can improve muscle strength, endurance, hypertrophy, bone density, metabolism and functional independence in CAD patients (Wise & Patrick 2011). Wise and Patrick add that regular resistance training improves exercise capacity, mood and quality of life. These resistance training recommendations come from the ASCM guidelines (2014):
- Equipment. Choose from free weights, wall pulleys, elastic bands, cuff and hand weights, and/or machines.
- Technique. Use slow, controlled movements; maintain regular breathing and do not hold the breath; avoid too much straining; avoid excessive gripping of weights.
- Intensity. Maintain light to somewhat hard exercise intensity, according to subjective assessment; this equates to an RPE of 11–14 on the 6–20 scale; use a 10- to 15-repetition zone of training.
- Frequency. Schedule two to three sessions per week.
- Number of exercises. Select eight to 10 exercises covering the major muscle groups of the body (chest, shoulders, abdominals, arms, back, hips, thighs, lower legs).
- Number of exercises in a session. Use a one-set-per-exercise design to train all muscle groups in a single session.
- Types of exercise. Include more multi-joint exercises that involve more muscle mass.
- Progression. Increase slowly in 2- to 5-pound increments for upper body and 5- to 10-pound increments for lower body, with progressions to be considered weekly.
- Number of sets. Begin with single-set training and progress to multiple-set regimens based on the client’s goals and ability to tolerate the additional exercise volume.
- Cautionary signs for early termination of workout. Watch for dizziness, lightheadedness, unusual shortness of breath, chest or shoulder pain/discomfort, which are all signs for the client to stop and seek medical assistance.
Final Thoughts
After a review and synthesis of the data, it is clear that well-structured cardiovascular exercise and resistance training programs are powerful therapeutic strategies for combating CAD. From regular participation in exercise, CAD clients may develop more confidence and self-esteem, work with greater vigor and, most importantly, enjoy life to its fullest. Fitness professionals have the research and tools to improve quality of life for CAD clients by designing individualized, safe and effective exercise programs.