
Are Pilates and Yoga Right for Clients With Low Bone Density?
After working with an older adult (aged 82–92) for 10 years, I was troubled to discover that she had begun having difficulty getting out of the waiting room chair before embarking on our weekly Pilates session. What was I missing? She had faithfully completed Reformer Footwork, Eve’s Lunge and Side Splits, as well as Standing Leg Pumps on the Wunda chair, each week. Why was she continuing to lose leg strength?
Upon further research, I learned that after age 50, adults typically lose about 1% of their leg strength and 0.5% of their bone mineral density (Gourlay et al. 2012) every year. If this doesn’t sound serious, consider that decreased leg strength—not dementia or incontinence—is the biggest predictor of loss of independence in older adults (Studenski et al. 2003).
There are ways to combat this seemingly inevitable decline, but do traditional Pilates and yoga programs make the grade? And if so, which exercises help, and which are contraindicated for clients whose bone density levels are already low?
Building Bone and Combating Falls
Science tells us that in order to build strength, we must overload targeted muscles beyond daily activity levels. To increase strength as opposed to endurance, fatigue must be reached in 8–12 repetitions. If 15–20 or more repetitions can be performed, endurance is improved, which does not build bone (Chahal, Lee
&
Luo 2014).
Muscle power (the ability to produce force rapidly) has emerged as a more crucial variable in functional decline than either muscle strength or muscle mass. In a community-based randomized controlled trial, Gianoudis and colleagues found that a targeted multimodal exercise program incorporating high-speed power training reduced falls and fracture risk factors in older adults (Gianoudis et al. 2014).
Apart from leg strength, which is crucial, key elements for maintaining independence and protecting against falls are balance; strength and mobility of the spine (especially the thoracic spine); and hip extension. Contraindicated moves for clients with (or at risk for) osteoporosis are spinal flexion and extremes of spinal rotation and side-bending.
Let’s review safety considerations that apply to clients with low bone density levels and then investigate whether Pilates or yoga can offer enough stimulation to improve key physical abilities without increasing a client’s risk of fracture.
Program Principles: Getting Started
A program for a client with either osteoporosis or osteopenia must focus above all on these five components:
-
fracture prevention—
most important!
- leg strength
- balance
- thoracic extension
- hip extension
All interventions for clients with low bone density should begin with an assessment (see the Web Extra for the top 10 tests). Enforcing a pre-exercise bone density test is not necessary. Occasionally, clients may lack health insurance or be unable to afford a test. Having no access to bone densitometry should not prohibit a client from beginning an exercise program that could reduce the risk of falls, fractures and loss of independence.
Even without a bone density study there are a few indicators that a client may have low bone mineral density:
- height loss greater than 1 inch
- presence of kyphosis
- family history
- previous fracture
Do not test spine mobility!
Before initiating an exercise program, teach the client to protect the spine, hip and ribs from fracture (see precautions below). Explain that focusing on fall prevention protects the wrists. Body awareness and education in principles of alignment will help the client to apply fracture prevention precautions in any exercise, sport or daily movement.
With or without the presence of a vertebral fracture, a client may safely begin an exercise program if you ensure that he or she observes the following precautions:
- Avoid rounding the spine when engaged in the activities of daily living.
- Exclude the following exercises:
- crunches
- sit-ups
- toe touches with round back
- forward bends with round back
- abdominal oblique work with rotation
- deep spinal side-bending (Avoid end range.)
- deep twists/spinal rotation (Avoid end range.)
- forced rotation of the femur, as in Pigeon pose
To identify beneficial exercises to include in a program, observe the client rising from a chair:
- Does the client use her hands to rise? This can indicate lower-extremity weakness.
- Do the client’s knees press together as he stands? This can indicate lower-extremity weakness and possibly lead to knee pain.
- Does the client round her back to stand? This can put the spine at risk for fracture.
- Can the client come to standing with good balance?
Pilates for Clients With Low Bone Density
The Pilates apparatus is designed mostly to
assist
people with movement, thus making everyday activities easier and more accessible. This sounds great at first, but “easier” does not meet the requirements for building strength.
Most Pilates mat exercises target core control and upper-body strength rather than lower-body strength and balance. In fact, only four mat moves work on leg strength: Shoulder Bridge, Side Bend, Leg Pull and Leg Pull Front.
The best overall Pilates mat exercise for osteoporosis is, ironically, Swimming! (See the Web Extra for more on how actual swimming and other types of exercise may negatively affect bone.) With its focus on extension and strengthening of the thoracic spine (with arms overhead for additional challenge) and on hip extension, Pilates Swimming is the ideal exercise for building bone in the spine (Bansal, Katzman
&
Giangregorio 2014) and possibly the hip (although the hip responds best to weight bearing). A pillow should always cushion the ribs during prone exercises.
Other good spinal-extension exercises are Swan, for increasing thoracic extension mobility; Double Leg Kick, for increasing thoracic extensor strength; Single Leg Kick, for core control and Push-Up preparation; and Leg Pull/Leg Pull Front, for upper- and lower-body strength as well as core control. Shoulder Bridge is excellent for hip extensor strength and spinal articulation.
Except for the mount to the Push-Up, the original mat repertoire from Joseph Pilates has no standing mat exercises (Pilates 1945). Therefore, any Pilates mat program needs to be supplemented with other leg-strengthening and balance exercises. Tai chi can be added to include balance and lower-extremity work for a well-rounded program (Hackney
&
Wolf 2014).
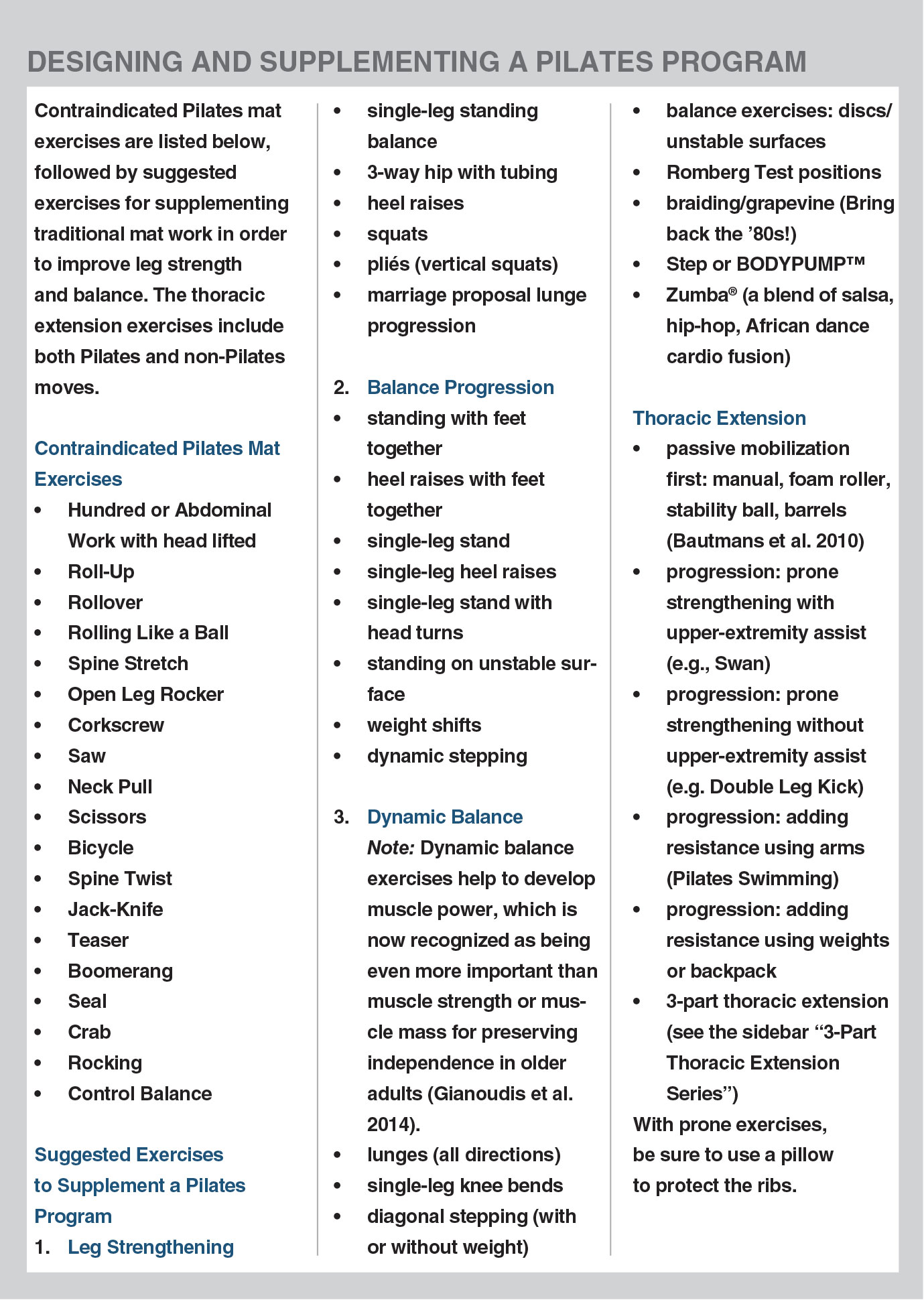
See the sidebar “Designing and Supplementing a Pilates Program” for important guidelines on working with Pilates clients.
Yoga for Clients With Low Bone Density
In yoga, practitioners coordinate breath with movement, holding poses for up to several minutes, depending on the style of yoga they are practicing. One main purpose of yoga is to allow the body to sit comfortably for meditation.
Yoga practices may focus on flexibility, strength, relaxation or flow. For bone health it is best to choose a practice that focuses on strength and proper biomechanical alignment. Greendale et al. (2009) conducted a randomized controlled trial comparing older-adult yoga participants with a control group and found that yoga students had less kyphosis after attending three yoga classes per week for 24 weeks.
For Pilates and yoga enthusiasts, yoga standing poses—often included as part of a vinyasa flow practice—may offer the best options for targeting leg strength, given the limited lower-body options in Pilates mat work. However, yoga also includes some very risky moves that can put bones at risk for fracture, adding to our conundrum.
Specifically, yoga practices often emphasize holding poses at end range while releasing into the position. This can be risky for those with low bone density, owing to the increased pressure on bones. At-risk participants may want to limit their movement to 75% of their joint range of motion while holding poses.
Spinal flexion is contraindicated for these participants (Sinaki
&
Mikkelsen 1984; Sinaki 2013; Betz 2005). (For more on the risks of flexion exercise, see my 2005 article in this journal, “Modifying Pilates for Clients With Osteoporosis” [Betz 2005].) Avoiding all spinal flexion and extremes of spinal rotation, side-bending and end-range hip motions will help to prevent fractures—the number-one priority with this population.
Sun Salutations are a great practice for building strength as long as students avoid spinal flexion during the transitions between poses. Emphasis on standing and balance poses rather than supine flexibility poses may also be good for stimulating bone. Poses that focus on thoracic extension, hip extension and balance are imperative for fracture prevention, posture, stride length during gait and possibly bone building. Less reliance on external props or support may help build balance, increase muscle strength and be beneficial in stimulating bone. When appropriate, however, poses can often be modified using a standard chair; for two examples, see the photographs of Runner’s Lunge and Warrior III.
For guidelines on which yoga poses are safe and which are not, see the sidebar “Designing a Safe Yoga Program.”
Summing Up
A well-rounded exercise program for osteoporosis should be varied, include dynamic movement and be performed in the best alignment possible. The fountain of youth is thoracic extension, hip extension, leg strength and balance. Safety is paramount, and remember, practice makes permanent!
2 Comments
Leave a Comment
You must be logged in to post a comment.
What about the reformer for osteoporosis ? I am 54 and have a lady which works with me on the reformer for core and uses the springs for the legs when I push off the board . I also do heavy weights with another trainer once a week . Time under load . Any advice is appreciated .
Add thoracic extension and balance to your workout Renee. Shoulder Bridge in neutral spine, Knee Stretches will open the hips and reinforce the Legs on the Reformer. Matwork: Leg Pull Front and Back, Swimming, Side Bend. On the Reformer The Long Box Serie: prone Side Pulls, Triceps extension, Swan, Swimming. Cadillac: Supine Arm Serie, Ladder Barrel Extension, Outside Cadillac: Squats, Prone in Arabesque: Shoulder mobilisation and Hip extension, etc…..