Unraveling the Stress- Eating-Obesity Knot
Elevated stress is a risk factor for cancer, high blood pressure and cardiovascular disease (Block et al. 2009). How stress influences eating behaviors and leads to obesity is a key topic of interest to researchers and exercise professionals.
A substantial amount of scientific research has been committed to unraveling this complex question. Block et al. submit that some people may gain more weight under stressful circumstances, while others may lose it and still others may have little change in weight. This article will summarize the state of knowledge regarding how stress can lead to higher food consumption, fat accumulation in the midsection, weight gain and obesity.
Stress
Torres and Nowson (2007) define stress as the nonspecific response of the body to any stimulus that overcomes, or threatens to overcome, the body’s ability to maintain homeostasis (the equilibrium of internal biological mechanisms). The authors explain that the stress response may be caused by social stressors (e.g., life events, personal conflicts); physiological stressors (e.g., pain, vigorous exercise, intense heat or cold); psychological or emotional stressors (e.g., sorrow, fear, anxiety); and/or chemical stressors (e.g., blood acid-base imbalance, low oxygen supply).
If the stressor represents an “ongoing” hassle, fear or overwhelming issue in a person’s life, the effect is referred to as chronic stress. In contrast, if the stressor is more temporary and immediate, the effect is referred to as acute stress. The body perceives an acute stressor (e.g., dealing with a traffic jam) as a challenge that a human being is capable of handling. On the other hand, chronic stress can seem unmanageable. Physiologically, the human body responds differently to acute and chronic stress.
The Body’s Response to Acute Stress
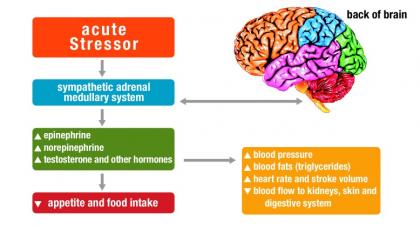
During periods of acute stress, the medullar part of the brain signals the release of several “stress hormones,” including epinephrine (another name for adrenaline) and norepinephrine (another name for noradrenaline) from the adrenal glands. These hormones trigger physiological “fight-or-flight” mechanisms, which include increases in heart rate, respiration rate, fat and carbohydrate breakdown, and blood pressure (see Figure 1). Simultaneously, the body slows down other physiological processes, such as blood flow to the digestive system, appetite and food intake. The body is priming itself with the immediate energy, reflexes and muscular strength it may need to act in response to the stressor. This is an automatic physiological response to a real or perceived risk that endangers a person’s present status. When the threat that triggered the response has been eliminated, the body and mind return to a state of calm.
The Body’s Response to Chronic Stress
With chronic stress, the hypothalamus (the central control station for stress) directs the pituitary gland (below the hypothalamus) in the brain to send a signaling message hormone (known as adrenocorticotrophic hormone, or ACTH) to the adrenal cortex (the outer portion of the adrenal glands on the kidneys). ACTH triggers the release of cortisol (see Figure 2) (Adam & Epel 2007). This reaction is referred to as the hypothalamic-pituitary-adrenocortical (HPA) axis, and it is most active in humans during the early-morning hours (Björntorp 2001).
If the chronic stress (real or perceived) is of sufficient magnitude and duration, the HPA does not wind down (as it should), resulting in prolonged elevation of cortisol levels. Thus, chronic stress leads to daily increases of cortisol secretion. Cortisol is known to stimulate appetite during the intermittent recovery periods that occur while a person is experiencing chronic stress. Cortisol (with the help of slightly elevated insulin levels) has also been shown to activate lipoprotein lipase, the enzyme that facilitates the deposition of fat (Björntorp 2001). In the presence of slightly higher insulin levels, elevated cortisol levels inhibit the breakdown of triglycerides, thus promoting fat storage. Epel et al. (2000) report that chronic stress consistently contributes to greater central fat accumulation in females.
Additionally, chronic stress is associated with emotional changes that can include increases in anxiety, apathy and depression (Torres & Nowson 2007). The response to chronic stress may lead to much higher consumption of food, referred to as stress-induced eating.
Stress-Induced Eating
Stress-induced eating may be defined as making oneself feel better by eating or drinking in response to a stressful situation (Torres & Nowson 2007). Greeno and Wing (1994) proposed two models of stress-induced eating. The first model, referred to as the general-effects model, predicts that stress will induce some type of psychological change that results in eating. The second, more commonly accepted model is referred to as the individual-differences model. This model suggests that owing to background learning, personal attitudes and biological differences, some people will change their eating habits under stressful conditions while others will not (see Figure 3).
Dallman (2010) asserts that in response to chronic stress and personal strains (e.g., interpersonal relationship, financial or lifetime aggravations), 40% or more of people will increase their caloric expenditure; 40% will decrease their caloric intake; and 20% will not change their eating behavior in any way. Consequently, stress-induced eating may be directly associated with weight gain and obesity for some people, but not for others.
Torres and Nowson add that during periods of chronic stress, people often have limited time to prepare healthy food choices and consequently tend to choose fast foods, which are usually more calorically dense. According to Dallman, the research suggests that overweight individuals tend to eat more when exposed to chronic stress, whereas normal-weight or underweight individuals do not. It appears that people who are chronically stressed—regardless of whether they eat more or less—tend to choose more pleasurable or palatable foods containing higher levels of fat and/or sugar (Dallman 2010).
Dallman adds that eating highly palatable foods temporarily decreases stress levels, which reinforces more eating of pleasurable foods. Thus, dealing with life’s stressors using food can become an incessant cycle that continues to contribute to obesity. Interestingly, Garg, Wansink and Inman (2007) note that when individuals who are in a saddened (or stressed) state read nutrition labels before eating, they indulge less in “hedonic” (pleasurable) foods.
The Buffering Effect of Exercise on Stress
The most comprehensive recent review on the health benefits of exercise and physical activity comes from the Physical Activity Guidelines Advisory Committee Report, 2008 published that year by the U.S. Department of Health and Human Services. In this exhaustive report, the section on mental health (part G, section 8) concludes that physical activity can protect against feelings of distress, defend against symptoms of anxiety, guard against depressive symptoms and the development of major depressive disorder and enhance psychological well-being. The document asserts that since 1995, more than 30 studies—involving more than 175,000 people—have been conducted in areas related to stress.
Although the measures of stress were not uniform in all of these research studies, the findings show with universal consistency that exercise interventions decrease stress levels and increase feelings of well-being. Dunn and Jewell (2010) add that exercise bouts of 30 minutes (but not longer than 60 minutes) appear to have the best “stress-reducing” benefits. There does not appear to be a differential effect based on the type of exercise (e.g., running, swimming, cycling, elliptical training, etc.). As to exercise intensity, the Physical Activity Guidelines report indicates that moderate to vigorous physical activity (with regular participation) reduces stress better than low-intensity activity.
The Neutralizing Effect of Mind-Body Programs on Stress
Astin et al. (2003) declare that the overall consensus of the pathophysiological and epidemiologic research suggests that acute and chronic stress contribute to the genesis of coronary artery disease. The authors add that an abundance of randomized, controlled studies since 1996 have shown that mind-body programs reduce the recurrence of myocardial infarctions (i.e., heart attacks) and other dangerous coronary events. After reviewing the literature on mind-body research, the authors concluded that integrating mind-body programs into traditional medical interventions should be considered a priority.
Final Thoughts
Stress sends biochemical “shock waves” throughout the body that are useful in the short term. However, chronic stress unleashes a flood of hormones that may become toxic as the stress persists. Exercise professionals need to educate their clients on the importance of exercise and mind-body practices in reducing the metabolic and physiological effects of stress and potentially lowering the risk of cardiovascular disease, hypertension and obesity. Science indicates that some of the best stress reduction strategies are exercise, relaxation activities, yoga and mind-body programs. In the long run, a decrease in stress can save the body from disease.
Source: Adapted from Torres & Nowson 2007.