Resistance Training and Diabetes: What’s Best?
Resistance training can be a big help to people who either have type 2 diabetes or are at risk of developing it. Ideally, trainers should combine cardiovascular and resistance training to help clients prevent or manage type 2 diabetes, but cardiovascular exercise isn’t always a good fit. In those cases, resistance training may be the only option available.
There’s no denying that diabetes is a serious health challenge. The World Health Organization (2015) estimates that 9% of adults worldwide have diabetes. Furthermore, 86 million Americans (more than 1 in 3) have prediabetes—an elevated risk of developing type 2 diabetes—and nearly 90% of them don’t know they have it (ADA 2016). Left untreated, 15%–30% of people with prediabetes will develop diabetes within 5 years (ADA 2016).
Fortunately, prediabetes can be reversed with exercise, weight loss and dietary changes (ADA 2016). This makes it imperative for fitness professionals to stay abreast of the most recent evidence-based exercise research to best prevent or manage type 2 diabetes.
Ishiguro et al. (2016) note that cardiovascular training is the traditional exercise for improving the metabolic profiles of patients with type 2 diabetes. These researchers say resistance training has gained a lot of attention recently because it can improve glycemic control, maintain bone mineral density, increase muscular strength and prevent osteoporosis. Unfortunately, Ishiguro et al. add, not all patients can get enough regular cardiovascular exercise to optimize health benefits. Thus, resistance training may be a first choice of exercise for some people with type 2 diabetes.
The Importance of Muscular Strength
Before we explore specific exercises for people who have type 2 diabetes or are at risk of developing it, we’ll review the biomechanical forces at work in this population.
The human skeletal-muscular system contains highly trainable tissue that can be remarkably effective in managing glycemic control, which in turn helps manage or prevent type 2 diabetes. Hurley, Hanson and Sheaff (2011) note that muscular strength is inversely related to metabolic syndrome, a cluster of risk factors leading to the development of type 2 diabetes and cardiovascular disease. The researchers add that high insulin levels, low muscle mass and low strength are the strongest factors associated with increased risk of metabolic syndrome.
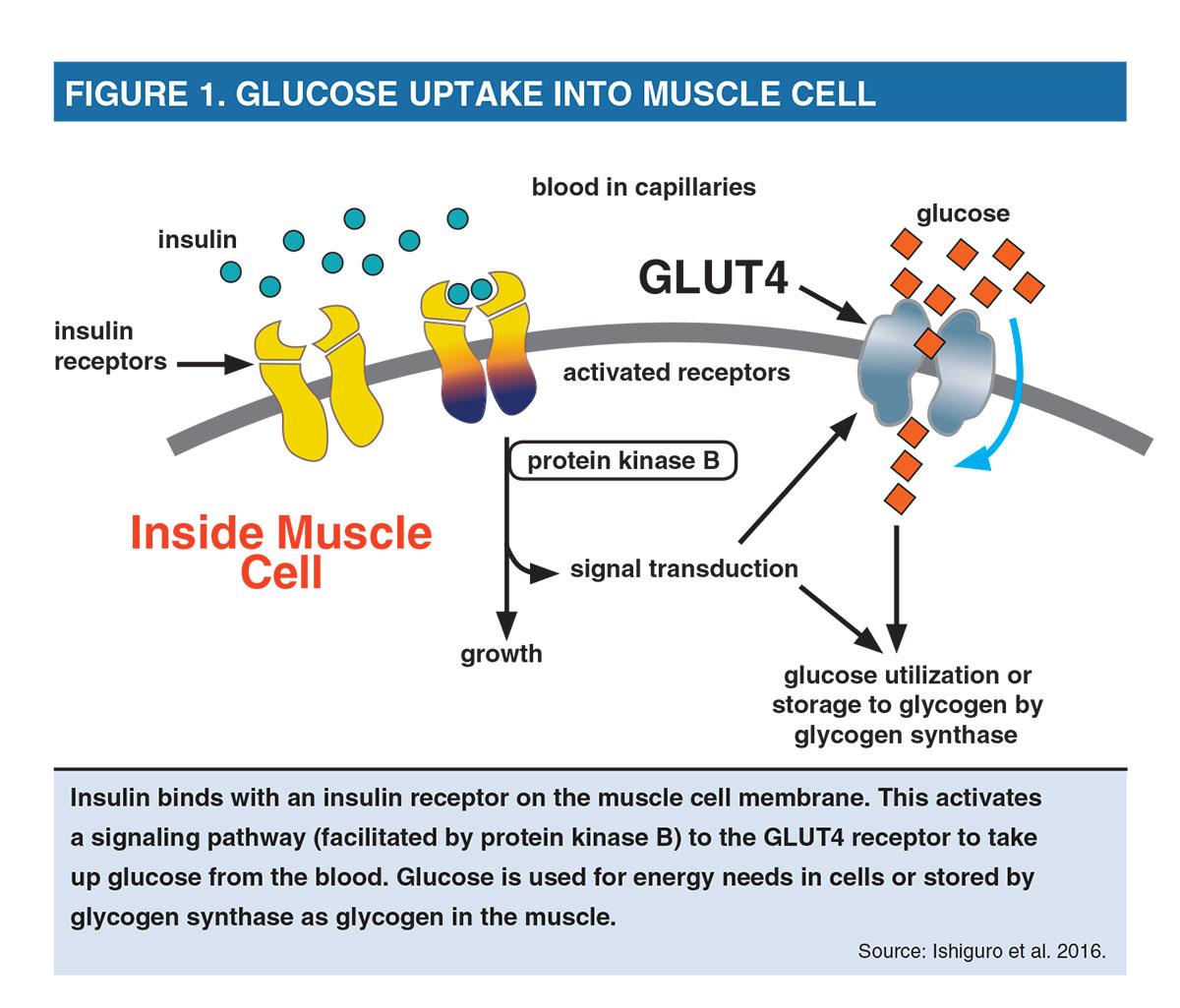
Ishiguro et al. (2016) explain that muscle contraction leads to a variety of muscle cell responses that ultimately enhance glucose uptake. Resistance exercise promotes glucose utilization by raising the number of glucose transporter-4 (GLUT4) proteins (transporter proteins taking glucose into muscle cells); by producing more insulin receptors; and by increasing the activity of protein kinase B (a signaling protein) and glycogen synthase (an enzyme involved in converting glucose to glycogen) (see Figure 1).
Muscle contraction reduces blood glucose concentrations and increases insulin sensitivity during and after exercise, with enhanced insulin sensitivity persisting for up to 24 hours (Colberg et al. 2010). Resistance exercise increases glucose uptake by upregulating (increasing the response to) the GLUT4 transporters, which can travel from within the cell to the membrane in response to muscle contraction (Gordon et al. 2009). The increased uptake moves glucose out of the blood and into the muscle, where it is used for energy needs or stored as glycogen for future exercise or work use.
Exercise Selection: Maximizing Activated Muscle Mass
Given that the glucose response is specific to the contracting muscles, Ishiguro et al. (2016) suggest focusing on exercises that will increase the muscle mass to be activated. To optimize glucose uptake, symptomatic people should do resistance exercises that engage large muscles and/or multiple muscle groups. The larger the muscle mass activated, the greater the potential for exercise-induced glucose uptake, because more GLUT4 transporters and insulin receptors will be stimulated.
Large, multijoint exercises such as chest press, shoulder press, latissimus dorsi pull-down, squat and dead lift are preferable to smaller, single-joint exercises such as chest fly, lateral shoulder raise and biceps curl. Total-body resistance training programs for both the upper and lower body have been shown to elicit significant effects on glucose clearance and insulin response in young and elderly people (Craig, Everhart
&
Brown 1989). To capitalize on this gain, personal trainers may wish to combine multijoint upper- and lower-body exercises into one movement to maximize engaged musculature.
Complex movements—including squat with shoulder press, lunge with biceps curl, and dead lift into upright row—may optimize the benefits of exercise-induced glucose control and make for time-efficient workouts, potentially increasing program adherence. Theoretically, these types of exercise could prove most effective for glycemic control.
From Theory to Application: Training Design to Best Manage Type 2 Diabetes
Ishiguro et al. (2016) suggest that two to three resistance training sessions per week may be optimal for improving people’s HbA1c levels (see the sidebar for how these levels are measured). The researchers note that more sessions per week don’t appear to have any greater benefit. Ishiguro and colleagues note that most studies on exercise and diabetes strive to progress resistance exercise intensities to 60%–80% of one-repetition maximum.
The effect of resistance training at higher intensities (
>
80% 1–RM) is not known. The data indicate that high-volume (multiset) training is almost certainly required to lower HbA1c levels. Ishiguro and colleagues say workout sessions need to build up progressively to 21 or more sets to meaningfully reduce HbA1c levels.
Final Takeaways
With the increasing prevalence of type 2 diabetes and insulin resistance, fitness professionals are likely at one time or another to have clients who are battling these health conditions. It is important to be armed with an arsenal of training tools to serve these clients and improve their health, particularly if they already have type 2 diabetes. Since activating muscle mass is a key goal with resistance training for glycemic control, personal trainers are encouraged to incorporate creative exercises that are multijoint and whole-body.
Clearly, a training program that is robust both in volume (21 or more sets per session) and in intensity (60%–80%) is a goal to progressively strive to attain. Most importantly, Sigal et al. (2007) highlight from their research that while either cardiovascular or resistance training alone improves glycemic control in type 2 diabetes, improvements are
greatest
when exercise programs combine resistance training and cardiovascular exercise.