Peripheral Heart Action Training: “What’s Old Is New Again”
If you have clients with high blood pressure or health problems that prevent them from using high-intensity interval training, then this study is for you.
The research explores peripheral heart action (PHA) training, a system of conditioning developed by Arthur Steinhaus, PhD, in the 1940s (Piras et al. 2015). PHA aims to keep blood circulating consistently during a resistance training session. Five to six exercises are performed sequentially at a medium intensity—with no rest between them; the exercises alter- nately stress upper- and lower-body muscles (Piras et al. 2015).
Interestingly, although PHA has been around for more than half a century, few people have investigated its effects on cardiovascular and autonomic function, the branch of the nervous system that controls internal organs and regulates heart rate, respiration and cardiac function. That changed last year, when Piras and colleagues compared the effects of PHA versus those of HIIT on cardiovascular and autonomic function in a group of young, untrained men and women. Let’s dig into the study’s particulars and look at the results.
Study Subjects
Eighteen healthy volunteers (9 women and 9 men, aged about 24, average BMI = 22.67) were randomly assigned to a HIIT group (8 subjects) or a PHA group (10 subjects). All of them were disease-free nonsmokers and were not taking prescription medications. Though the participants were recreationally active, they were untrained. Their maximal aerobic capacity averaged 32.89 milliliters per kilogram of body weight per minute, a “poor” classification for their age and gender.
Study Methods
All volunteers did pre- and post-tests within 3–4 days of the 3-month training period, which consisted of three exercise sessions per week, separated each time by 1–2 days of rest. Study researchers supervised all training sessions. Muscular strength assessments used one-repetition maximum testing on the pectoralis major and minor, quadriceps, latissimus dorsi, hamstrings, deltoids and gastrocnemius. Autonomic function tests measured heart rate variability (the physiological variation in the time interval between heartbeats) and baroreflex sensitivity (a measure of the interaction between sympathetic and parasympathetic activ- ities that directly affect cardiac health).
HIIT Training Group
The HIIT group completed a 5-minute warm-up on a cycle ergometer and began HIIT training with a 1-minute, high-intensity work bout at the level of their maximal aerobic capacity, followed by a 2-minute recovery interval (no load on the cycle). Work and recovery intervals were performed 5 times, with a 5-minute cool-down at the end of the workout.
PHA Training Group
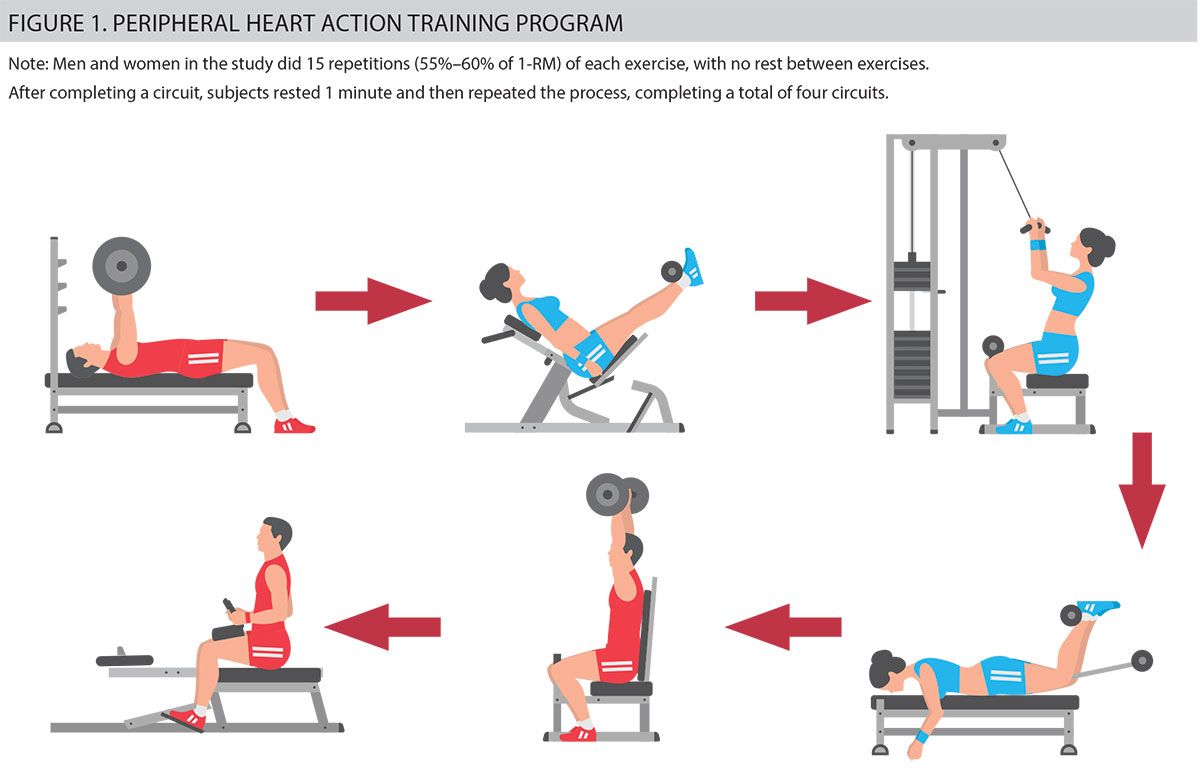
Each PHA session began with a 5-minute warm-up and concluded with a 5-minute cool-down. The PHA protocol used six exercises strictly ordered in this circuit sequence: pectoralis major, leg extension, latissimus dorsi pull-down, leg curl, shoulder press and calf machine (see Figure 1). There was no rest between exercises.
All subjects completed 15 repetitions of each exercise at 55%–60% of their 1-RM. After completing the first circuit,
they rested 1 minute and then repeated the process in identical fashion until they had done four circuits. Subjects wore heart rate monitors during the PHA training, which held heart rates consistently at 60%–80% of maximal heart rate (calculated from the maximal aerobic capacity pretest).
Study Results
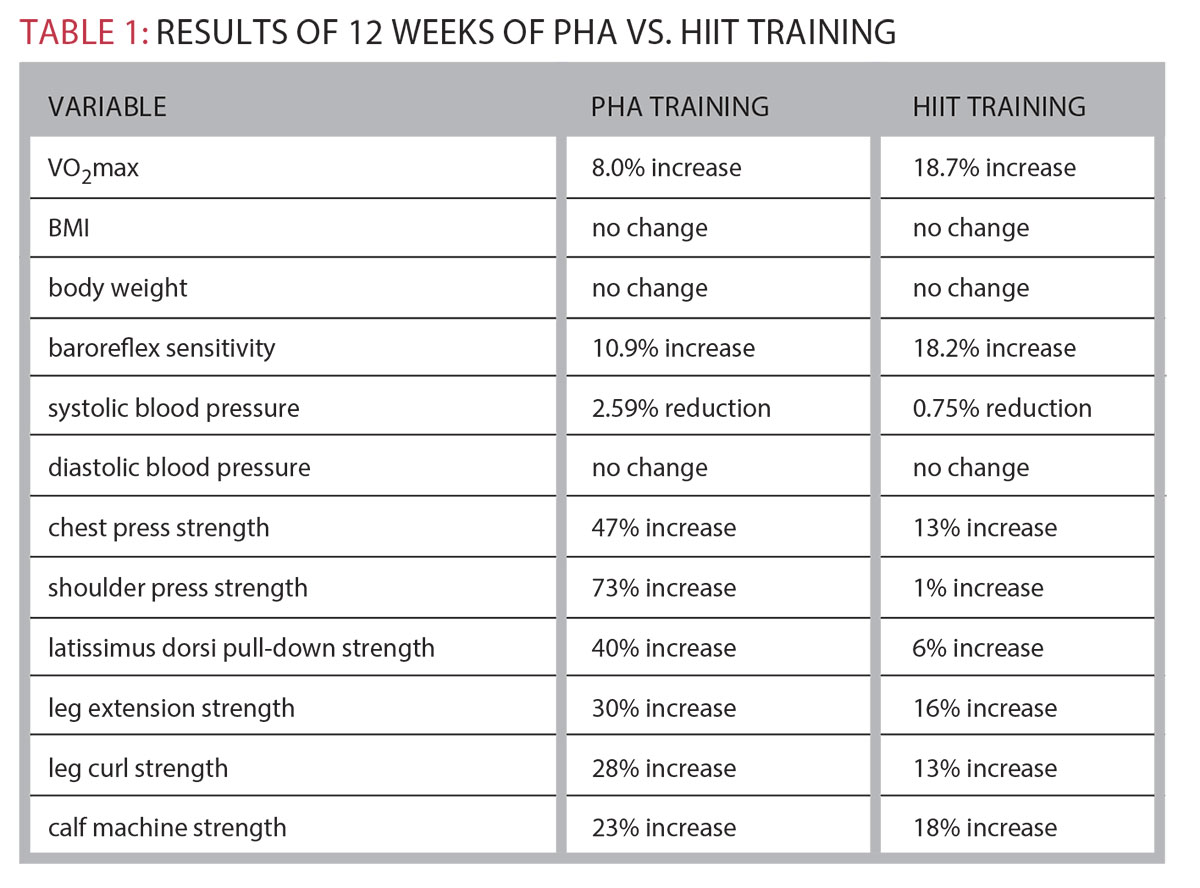
This research is the first longitudinal 12-week study to complete such an exhaustive analysis of PHA training in comparison with HIIT training. Table 1 synthesizes many of the study results. Most interestingly, the improvement in maximal aerobic capacity for PHA is higher than that reported in traditional circuit training studies. The PHA concept of alternating upper-and lower-body exercises, performed at a medium exercise intensity (with no rest between exercises), stimulates several variables of cardiovascular function.
Piras and colleagues hypothesize that PHA training provides the appropriate stress for the cardiovascular system to adapt. They believe this type of exercise may increase peripheral blood flow (i.e., in the arms, hands, legs and feet) during the training and improve cellular metabolic activity.
With PHA, the heart rate variability markers of autonomic activity (controlling heart rate) were reduced. These results indicate a very positive response for improving heart health, and they were more favorable in the PHA group than in the HIIT group. The baroreflex sensitivity markers also showed encouraging improvement in the 12-week study, for both groups.
As expected, the PHA group showed much better muscular strength improvements in lower-and upper-body musculature than the HIIT group.
Piras et al. note that these findings may prove most beneficial for the prevention or management of metabolic syndrome, obesity, sarcopenia and osteoporosis.
In 12 weeks, PHA training produced meaningful reductions in systolic blood pressure—scoring better than HIIT training. Piras et al. (2015) propose that PHA training should be considered a viable option for people with elevated blood pressure or with clinical pathology health conditions that do not allow them to train at high intensities.
The researchers suggest that combining HIIT training with PHA may very likely have even greater benefits for reducing elevated blood pressure in people with hypertension.
Is There a Physiological Mechanism at Work With PHA Training?
There is no rest between sets with PHA, and the exercises alternate between upper body and lower body. In 1978, Asmussen & Mazin showed that more dynamic work can be accomplished by exercising continuously across different muscle groups instead of resting between exercises. Piras et al. (2015) propose that with blood flow continuously increasing during a PHA training session, PHA may very likely be the more effective way to remove the metabolites (i.e., hydrogen ions and carbondioxide)thatcontributetofatigue.
What’s Old Is New Again
The results of this study are most impressive. PHA training promotes positive adaptations in several variables related to
cardiovascular function, blood pressure and autonomic regulation. The improvements in heart rate variability and barometric sensitivity are associated with less
risk for all causes of mortality and morbidity. All of these improvements translate into greater protection from cardiovascular disease. In addition, the muscular strength gains of this type of training are quite impressive. What’s old is new again, and this new, promising research suggests that PHA training is going to be around for quite some time.