Diabetes & Exercise: What Every Fitness Professional Should Know
Diabetes affects nearly one-tenth of the U.S. population—a widening epidemic with more than 5,000 new cases per day and an economic cost of $245 billion per year (ADA 2013).
These alarming statistics and their worrisome health consequences (see Figure 1) make it imperative for us to understand how to manage or prevent diabetes safely and effectively. Fortunately, research demonstrates that regular exercise may combat some of the deleterious effects of diabetes and can sometimes prevent it from striking high-risk individuals (Colberg et al. 2010). Colberg et al. say studies find that exercise supervised by qualified trainers has the greatest impact on controlling blood glucose—the pivotal factor in all diabetes cases. That’s why it’s so important for certified exercise professionals to take the lead in educating clients on the risks, management and deterrence of diabetes.
Historical Roots of Diabetes and Insulin
The combined symptoms of rapid weight loss, extreme thirst and constant urination have confronted medical practitioners for more than 3,000 years. The term diabetes, Greek for “to pass through,” was first used by Apollonius of Memphis in 230 bc (Zajac et al. 2010). Aretaeus of Cappadocia, a Greek physician in the second century ad, helped to clarify diabetes symptoms (excessive thirst and urination; also see Figure 2) and outcomes (shorter life) (Zajac et al. 2010).
Attempts to treat diabetes failed for millennia, though doctors did come to understand that the disease had something to do with blood glucose. The biggest breakthroughs happened after Frederick Grant Banting and Charles Best from Canada were credited with discovering the efficacy of insulin in 1921, leading to many treatment and research advances (Zajac et al. 2010). Banting and Best created a pancreatic extract that improved the condition of diabetic dogs. In 1922, the two scientists injected the first human subject, a 14-year-old diabetic boy, with a variety of the extract that came to be called insulin. Within 24 hours, the boy’s blood glucose plunged from a dangerously high 520 milligrams per deciliter to 120 mg/dL, which is just above normal in nondiabetics (Zajac et al. 2010). That same year, insulin was purified and commercially produced by Eli Lilly Company, which worked closely with Banting and Best (Zajac et al. 2010).
What Are the Varieties of Diabetes?
Diabetes has three main types: type 1, type 2 and gestational. Prediabetes is not a distinct type, though it is sometimes characterized as a precursor that indicates an increased risk of developing type 2 diabetes.
Type 1
Type 1 diabetes, formerly called juvenile-onset diabetes, accounts for 5%–10% of all diabetes cases (Colberg et al. 2010). Type 1 is an autoimmune disease where the body’s defense system mistakenly attacks the pancreatic islet beta cells that produce insulin (IDF 2014), totally depleting the body’s insulin secretions. To survive, type 1 diabetics need daily insulin injections or an insulin pump to control their blood glucose levels. Type 1 diabetes is usually diagnosed in children or young adults, yet it may affect people at any age. A type 1 diabetes intervention is built on creating a healthy lifestyle with increased physical activity, a healthy diet, weight control and proper insulin medication.
Type 2
Type 2 diabetes, formerly called non-insulin-dependent diabetes or adult-onset diabetes, accounts for about 90% of diabetes cases (IDF 2014). It is described as a condition of insulin resistance, which means the body is misusing the insulin the pancreas produces (see “What Is the Pathophysiology of Type 2 Diabetes?”). As blood glucose levels rise in a type 2 patient, the body’s cells become unable to take up the extra glucose. A diagnosis of type 2 diabetes may occur at any age. Insulin resistance and type 2 diabetes are highly associated with overweight and/or obesity (IDF 2014). People with type 2 diabetes can manage their condition by exercising, following a healthy meal plan, losing excess weight and taking oral medications (Colberg et al. 2010).
Gestational
Gestational diabetes mellitus (GDM) is a form of diabetes in which high blood glucose levels develop during pregnancy. It occurs once in every 25 pregnancies worldwide, with complications to both mother and baby (IDF 2014). GDM usually disappears after pregnancy, but women with GDM and their children have an increased risk of developing type 2 diabetes later in life. Furthermore, about half of women with a history of GDM develop type 2 diabetes within 5–10 years after delivery (IDF 2014).
Prediabetes
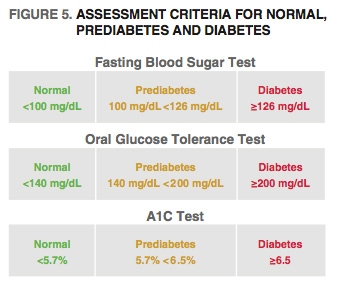
People with prediabetes have impaired fasting glucose or impaired glucose tolerance—or both. With the former, the fasting blood sugar level is 100–125 mg/dL after an overnight fast—higher than normal (75–100 in nondiabetics), but too low to be classified as diabetes. With the latter, the blood sugar level is 140–199 mg/dL after a 2-hour oral glucose tolerance test, which is also above normal but not high enough to be classified as diabetes (ADA 2014a).
What Is the Pathophysiology of Type 2 Diabetes?
Because diet and exercise can play a large role in treating or preventing type 2 diabetes, it’s helpful to understand the role of blood glucose regulation in the hormonal pathophysiology that leads to this variety of the disease. Glucose, a simple sugar from carbohydrates, is a primary fuel that the body’s cells break down to liberate energy for life, work and exercise. The body stores glucose in the form of glycogen in muscle and the liver, and regulates glucose levels with insulin and glucagon, two hormones secreted by the pancreas.
Insulin and glucagon are made by specialized islets of Langerhans cells, named after the German physician Paul Langerhans, who described them in 1869 (Ruder 2011). Islet beta cells create insulin, which helps the body uptake glucose from the blood (Ruder 2011). Islet alpha cells produce glucagon, which stimulates the liver to raise glucose levels if they are low (Ruder 2011). Normal glucose regulation involves a complex interplay of insulin, glucagon and circulating glucose to maintain a homeostatic balance (see Figure 3).
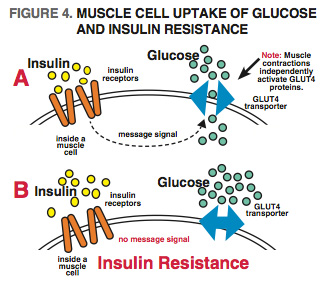
Normally, insulin binds to insulin receptors on the muscle cells that signal glucose transporters known as GLUT4 proteins to shuttle glucose into the cells (Ploug & Ralston 2002) (see Figure 4). Disruptions to this process prevent glucose from being deposited into the cells, which causes blood glucose levels to rise—the condition called insulin resistance (see Figure 4).
High blood glucose levels cause the pancreas to produce more insulin, which creates an excess in the blood stream. Eventually, type 2 diabetes presents if nothing is done to rectify this impaired metabolic imbalance of elevated glucose and insulin.
What Are the Main Risk Factors for Developing Type 2 Diabetes?
The American Diabetes Association (ADA 2014a) has established the following risk factors for type 2 diabetes:
- adults who are overweight (BMI ≥25 kg/m2) and have additional risk factors from this list
- physical inactivity
- first-degree relative with diabetes
- high-risk race/ethnicity (such as African American, Latino, Native American, Asian American, Pacific Islander)
- women who have delivered a baby weighing more than 9 pounds or were diagnosed with gestational diabetes
- hypertension (140/90 mm Hg or on therapy for hypertension)
- HDL cholesterol level <35 mg/dL (0.90 mmol/L) and/or a triglyceride level >250 mg/dL (2.82 mmol/L)
- women with polycystic ovarian syndrome
- A1C ≥5.7%, impaired glucose tolerance or impaired fasting glucose on previous testing
- other clinical conditions associated with insulin resistance (such as severe obesity and acanthosis nigricans—a skin disorder in which there is darker, thick, velvety skin in body folds)
- history of cardiovascular disease
Note: In the absence of the above criteria, testing for diabetes should begin at age 45. If results are normal, testing should be repeated at least every 3 years, with consideration of more frequent testing depending on initial results and risk status (those with prediabetes should be tested yearly).
How Is Diabetes Diagnosed?
Healthcare professionals use several tests based on plasma glucose criteria to diagnose prediabetes or diabetes. The fasting blood glucose test measures blood glucose after an 8-hour fast. The oral glucose tolerance test measures blood glucose 2 hours after consumption of a glucose-laden drink (75 g of glucose). One of the preferred tests measures hemoglobin A1C, which reflects average blood glucose over 2–3 months.
If a test result exceeds the diagnostic cut point, the test is repeated to rule out lab error, unless the diagnosis is clear, as may happen, for example, when a person displays classic symptoms of hyperglycemia (ADA 2014b). If a person’s results are above the criterion level in one test and normal in another, the test with the elevated result is repeated. Criteria levels for normal, prediabetes and diabetes are shown in Figure 5.
What Are the Management Goals for Type 2 Diabetics?
The major focus of managing type 2 diabetes is to protect against the long-term complications of the disease. Since insulin resistance is a key player in type 2 diabetes, which also influences cardiovascular disease, interventions focus on improving insulin sensitivity by enhancing glucose uptake. Lifestyle interventions, healthy eating, exercise, weight loss, self-care behaviors and oral medications are all considered (ADA 2014a).
Centerpieces of most type 2 diabetes management plans are exercise and diet, because they improve glucose metabolism, blood lipids and blood pressure abnormalities, and contribute to sustained weight loss (Colberg et al. 2010). Colberg et al. propose that medications should complement lifestyle improvements, not replace them.
What Are the Metabolic Effects of Exercise?
During exercise, the most important factors influencing fuel use are intensity and duration (Colberg et al. 2010). Muscle glycogen provides plenty of fuel for working muscles, but as those stores are depleted with increased intensity, muscles increase their uptake and utilization of circulating blood glucose and free fatty acids (Colberg et al. 2010).
The breakdown of stored glycogen is called glycogenolysis. Even in the presence of type 2 diabetes, blood glucose uptake by working muscles is normal because muscle contractions trigger GLUT4 transporters (also called translocators) (Colberg et al.
2010). Colberg and colleagues note that this independent muscle contraction–mediated uptake of blood glucose remains elevated for several hours, a very noteworthy benefit of exercise. Type 2 diabetes impairs insulin-stimulated GLUT4 translocation, which is why exercise is so vital. Importantly, resistance exercise and aerobic training increase GLUT4 abundance and blood glucose uptake (Colberg et al. 2010).
Recent research has shown that resistance exercise is as important as, and perhaps even more important than, aerobic training in diabetes management (Colberg et al. 2010). An increase in muscle mass resulting from resistance training can contribute profoundly to glucose uptake. However, a combination of aerobic exercise and resistance training is more effective for blood glucose control than either type of exercise alone (Colberg et al. 2010).
Physical activity of any intensity will provide acute effects by enhancing blood glucose uptake for glycogen synthesis and by stimulating fat oxidation (breakdown) in muscle (Colberg et al. 2010). Colberg and colleagues add that current research suggests that longer-duration and more-intense training sessions elicit the best results for blood glucose reductions.
In educating clients on preventing or managing diabetes, personal trainers need to stress the importance of aerobic exercise and resistance training, because both improve long-term insulin action, blood glucose control and fat oxidation in muscle (Colberg et al. 2010). Trainers should encourage clients to achieve higher levels of physical fitness and physical activity, as they are associated with lower rates of cardiovascular disease and mortality in both healthy and diabetic patients (Colberg et al. 2010).
Preexercise Evaluation
Diabetes-related health complications like cardiovascular disease, hypertension, neuropathy (nerve damage) and microvascular changes (i.e., changes to small blood vessels) can complicate safe exercise participation. For those planning low-intensity activity, such as walking, conducting an exercise stress test before starting is unnecessary. Requiring these people to do a stress test may discourage them from participating (Colberg et al. 2010).
Sedentary and older diabetics who plan to engage in activities more intense than brisk walking should be assessed before they start. Conditions of concern include uncontrolled hypertension, severe autonomic neuropathy (damage to nerves that control body functions such as blood pressure, heart rate, sweating, bowel and bladder emptying, and digestion), severe peripheral neuropathy (affecting nerves outside the brain and spinal cord), history of foot lesions, and unstable proliferative retinopathy (growth of new blood vessels on retina that can bleed).
The client’s age and previous physical activity level should be considered. People with complications may require a more thorough evaluation by a qualified health practitioner.
Summary Thoughts
Exercise professionals can make a major difference in helping clients prevent or manage diabetes. Colberg et al. (2010) stress that combining aerobic exercise with resistance training is the best way to enhance blood glucose control. The authors also recommend that clients increase their daily unstructured movement (spontaneous physical activity), as this will increase caloric expenditure and contribute to weight loss goals.
Personal trainers are advised to help their diabetic clients monitor blood glucose before, during and after exercise. With higher-intensity exercise programs, which elevate metabolism for hours after exercise, clients with diabetes are also encouraged to check their blood glucose a few hours after exercise (and even before going to sleep) and to have a snack if glucose falls below 100 mg/dL. Cardiovascular exercise and resistance training are persuasive pillars for the prevention and treatment of type 2 diabetes. Let’s combat this disease now!